Definition of Xeroderma
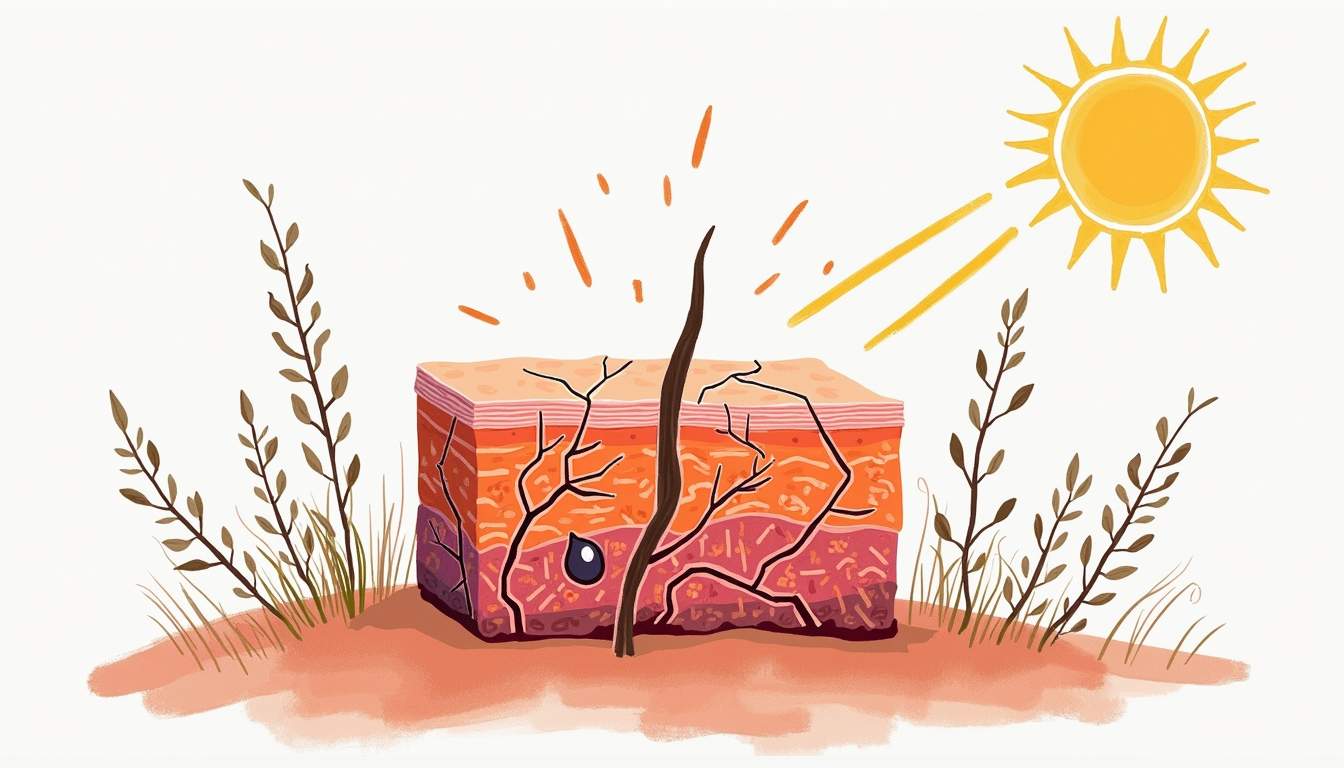
Xeroderma, commonly referred to as dry skin, is a dermatological condition characterized by the excessive dryness of the skin. This condition can manifest in various forms, ranging from mild dryness to severe scaling and cracking. Xeroderma is not merely a cosmetic issue; it can lead to discomfort, itching, and even more serious skin complications if left untreated. The term 'xeroderma' is derived from the Greek words 'xero,' meaning dry, and 'derma,' meaning skin. This condition can affect individuals of all ages and backgrounds, although certain populations may be more susceptible due to genetic predispositions or environmental factors.
In dermatology, xeroderma is often categorized based on its etiology, which can include intrinsic factors such as genetics and age, as well as extrinsic factors like environmental conditions and lifestyle choices. Understanding the underlying causes of xeroderma is crucial for effective management and treatment. The skin serves as a barrier to protect the body from external elements, and when it becomes dry, that barrier function is compromised, leading to potential health risks.
Furthermore, xeroderma can be a symptom of various underlying health conditions, including atopic dermatitis, psoriasis, and even systemic diseases. Therefore, it is essential for healthcare providers to conduct a thorough assessment to determine the root cause of xeroderma in each patient. This comprehensive approach ensures that treatment is tailored to the individual's specific needs and circumstances.
Causes of Xeroderma
Intrinsic Factors
Intrinsic factors contributing to xeroderma include genetic predispositions, age, and hormonal changes. Genetic conditions such as ichthyosis can lead to abnormal skin cell turnover, resulting in excessively dry skin. As individuals age, the skin naturally loses moisture and elasticity, which can exacerbate the symptoms of xeroderma. Hormonal changes, particularly during menopause, can also lead to decreased oil production in the skin, further contributing to dryness.
Additionally, certain medical conditions can predispose individuals to xeroderma. For instance, diabetes can lead to dry skin due to poor circulation and nerve damage, while thyroid disorders can affect skin hydration levels. Understanding these intrinsic factors is vital for dermatologists to provide effective treatment options and lifestyle recommendations.
Extrinsic Factors
Extrinsic factors encompass environmental influences and lifestyle choices that can contribute to xeroderma. Environmental conditions such as low humidity, extreme temperatures, and exposure to harsh winds can strip the skin of its natural moisture. Individuals living in arid climates or those who frequently use air conditioning or heating systems are particularly vulnerable to developing xeroderma.
Moreover, lifestyle choices such as frequent bathing, especially with hot water, can exacerbate skin dryness. The use of harsh soaps and detergents can further compromise the skin's natural barrier, leading to increased transepidermal water loss. Occupational exposure to irritants, such as chemicals or prolonged water exposure, can also play a significant role in the development of xeroderma.
Symptoms of Xeroderma
Common Symptoms
The symptoms of xeroderma can vary widely among individuals, but common manifestations include rough, flaky skin, tightness, and a feeling of discomfort. The skin may appear dull and lack the natural glow associated with healthy skin. In more severe cases, xeroderma can lead to cracking and fissuring, particularly in areas such as the hands, feet, and elbows. These cracks can be painful and may become infected if not properly managed.
Itching is another prevalent symptom associated with xeroderma, which can lead to scratching and further damage to the skin. This cycle of itching and scratching can create a vicious cycle, exacerbating the condition and leading to secondary infections. In some cases, individuals may also experience redness or inflammation in the affected areas, indicating an underlying inflammatory response.
Severe Symptoms
In severe cases of xeroderma, individuals may experience widespread skin changes that can significantly impact their quality of life. The skin may become so dry that it leads to dermatitis, a condition characterized by inflammation, redness, and swelling. This can further complicate the management of xeroderma and may require more intensive treatment approaches.
Additionally, xeroderma can lead to complications such as skin infections, particularly if the skin barrier is compromised. Bacterial or fungal infections can occur in areas of broken skin, necessitating prompt medical intervention. Chronic xeroderma can also contribute to the development of skin conditions such as eczema or psoriasis, which may require specialized dermatological care.
Diagnosis of Xeroderma
Clinical Evaluation
The diagnosis of xeroderma typically begins with a thorough clinical evaluation by a dermatologist. During this evaluation, the healthcare provider will assess the patient's medical history, including any underlying health conditions, medications, and lifestyle factors that may contribute to skin dryness. A physical examination of the skin will also be conducted to evaluate the extent and severity of xeroderma.
In some cases, additional diagnostic tests may be warranted to rule out underlying conditions that could be contributing to xeroderma. These tests may include skin biopsies, blood tests, or allergy testing, depending on the clinical presentation and suspected etiology. A comprehensive approach to diagnosis ensures that the underlying causes of xeroderma are identified and addressed appropriately.
Differential Diagnosis
It is essential to differentiate xeroderma from other dermatological conditions that may present with similar symptoms. Conditions such as eczema, psoriasis, and contact dermatitis can all lead to dry, irritated skin, but they may require different treatment approaches. A dermatologist will consider the patient's history, symptoms, and clinical findings to arrive at an accurate diagnosis.
For example, eczema is often associated with intense itching and may have a genetic component, while psoriasis is characterized by well-defined plaques and may have a systemic component. Understanding these differences is crucial for effective management and treatment of xeroderma and its associated conditions.
Treatment Options for Xeroderma
Moisturizers and Emollients
The cornerstone of xeroderma management is the regular use of moisturizers and emollients. These products work by creating a barrier on the skin's surface, preventing moisture loss and enhancing hydration. It is essential to choose the right type of moisturizer based on the severity of xeroderma. For mild cases, lightweight lotions may suffice, while more severe cases may require thicker creams or ointments that provide a more occlusive barrier.
When selecting moisturizers, individuals should look for products that contain ingredients such as glycerin, hyaluronic acid, and ceramides, which are known for their hydrating properties. Additionally, occlusive agents like petrolatum or dimethicone can help lock in moisture and protect the skin from environmental irritants. Regular application of moisturizers, ideally after bathing, can significantly improve skin hydration and alleviate symptoms of xeroderma.
Topical Treatments
In some cases, dermatologists may recommend topical treatments to address underlying inflammation or irritation associated with xeroderma. Corticosteroid creams can be effective in reducing inflammation and itching, particularly in cases where xeroderma is accompanied by dermatitis. However, these should be used judiciously and under the guidance of a healthcare provider to avoid potential side effects.
Other topical treatments may include keratolytic agents, which help to exfoliate dead skin cells and improve skin texture. Ingredients such as urea or salicylic acid can be beneficial in cases of severe scaling or thickened skin. It is essential to follow a dermatologist's recommendations regarding the use of these treatments to ensure safety and efficacy.
Prevention of Xeroderma
Lifestyle Modifications
Preventing xeroderma involves a combination of lifestyle modifications and skincare practices. Individuals should aim to maintain a consistent skincare routine that includes regular moisturizing, especially after bathing or washing hands. Using lukewarm water instead of hot water during showers can help preserve the skin's natural oils and prevent excessive drying.
Additionally, individuals should be mindful of their environment. Using a humidifier in dry indoor spaces can help maintain moisture levels in the air, reducing the risk of xeroderma. Wearing protective clothing in extreme weather conditions, such as gloves in cold weather or sunscreen in sunny conditions, can also help shield the skin from environmental stressors.
Diet and Hydration
Dietary choices can also play a significant role in skin health. Consuming a balanced diet rich in essential fatty acids, vitamins, and antioxidants can support skin hydration and overall health. Foods such as avocados, nuts, seeds, and fatty fish are excellent sources of omega-3 fatty acids, which can help improve skin barrier function.
Staying adequately hydrated is equally important for maintaining skin moisture levels. Drinking sufficient water throughout the day can help keep the skin hydrated from the inside out. Limiting the intake of dehydrating substances such as alcohol and caffeine can also contribute to better skin health.
Conclusion
Xeroderma is a common dermatological condition that can significantly impact an individual's quality of life. Understanding the causes, symptoms, and treatment options for xeroderma is crucial for effective management. By adopting a comprehensive approach that includes lifestyle modifications, proper skincare, and medical interventions when necessary, individuals can effectively manage xeroderma and maintain healthy, hydrated skin.
As with any dermatological condition, it is essential to consult with a qualified healthcare provider for personalized recommendations and treatment options. Early intervention and proactive management can help prevent complications and ensure optimal skin health.
Visit Our Offices
Services:
- • Medical Dermatology
- • Surgical Dermatology
- • Laser Treatments
- • Cosmetic Dermatology
Services:
- • Medical Dermatology
- • Surgical Dermatology
- • Laser Treatments
- • Cosmetic Dermatology
Visit Our Offices
Services:
- • Medical Dermatology
- • Surgical Dermatology
- • Laser Treatments
- • Cosmetic Dermatology
Services:
- • Medical Dermatology
- • Surgical Dermatology
- • Laser Treatments
- • Cosmetic Dermatology