Introduction to Psoriasis
Psoriasis is a chronic autoimmune condition characterized by the rapid proliferation of skin cells, leading to the formation of scaly, inflamed patches on the skin. It is a common skin disorder that affects millions of people worldwide, manifesting in various forms and severities. The condition is not merely a cosmetic issue; it can significantly impact the quality of life, causing physical discomfort and emotional distress.
Understanding psoriasis requires a multifaceted approach that encompasses its pathophysiology, clinical manifestations, treatment options, and the psychosocial implications it carries. This glossary entry aims to provide a comprehensive overview of psoriasis, elucidating its complexities and the latest advancements in dermatological care.
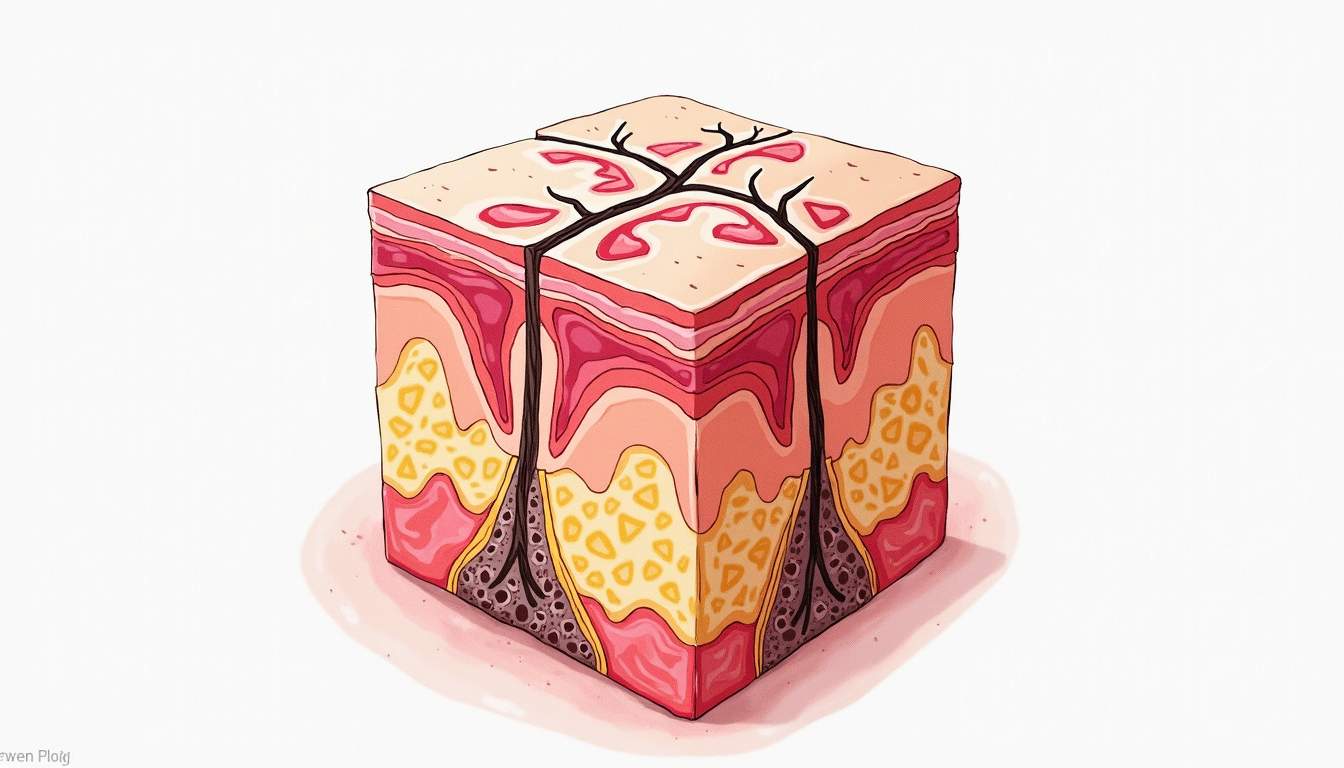
Pathophysiology of Psoriasis
Immune System Involvement
At the core of psoriasis is an aberrant immune response. The immune system mistakenly attacks healthy skin cells, leading to an inflammatory cascade. T-cells, a type of white blood cell, play a pivotal role in this process. When activated, these T-cells release pro-inflammatory cytokines, such as tumor necrosis factor-alpha (TNF-alpha) and interleukins (IL-17, IL-23), which further stimulate the proliferation of keratinocytes, the predominant cell type in the epidermis.
This hyperproliferation results in the characteristic thickened plaques seen in psoriasis. The rapid turnover of skin cells means that they do not have enough time to mature properly, leading to the accumulation of dead skin cells on the surface, which forms the silvery scales typical of the condition.
Genetic Factors
Genetics also play a crucial role in the development of psoriasis. Studies have identified several susceptibility loci associated with the disease, indicating a hereditary component. Individuals with a family history of psoriasis are at a higher risk of developing the condition, suggesting that genetic predisposition, combined with environmental triggers, contributes to its onset.
Research has shown that certain genes involved in immune response regulation and skin barrier function are often altered in individuals with psoriasis. These genetic factors can influence the severity of the disease and the response to treatment, highlighting the importance of personalized medicine in managing psoriasis.
Clinical Manifestations
Types of Psoriasis
Psoriasis can manifest in several distinct forms, each with unique characteristics. The most common types include:
- Plaque Psoriasis: The most prevalent form, characterized by raised, red patches covered with silvery-white scales. These plaques are often itchy and can appear anywhere on the body, although they are commonly found on the elbows, knees, and scalp.
- Guttate Psoriasis: Often triggered by bacterial infections, this type presents as small, drop-shaped lesions primarily on the trunk and limbs. It is more common in children and young adults.
- Inverse Psoriasis: This form occurs in skin folds, such as under the breasts, in the groin, or around the armpits. It appears as smooth, red patches without the typical scaling.
- Pustular Psoriasis: Characterized by white pustules (blisters of non-infectious pus) surrounded by red skin. It can be localized or generalized and may be accompanied by systemic symptoms.
- Erythrodermic Psoriasis: A severe and rare form that leads to widespread redness and shedding of the skin over large areas of the body. It can be life-threatening and requires immediate medical attention.
Symptoms and Complications
The symptoms of psoriasis can vary significantly from person to person, depending on the type and severity of the disease. Common symptoms include:
- Red patches of skin covered with thick, silvery scales.
- Dry, cracked skin that may bleed.
- Itching, burning, or soreness.
- Thickened, pitted, or ridged nails.
- Swollen and stiff joints, indicating psoriatic arthritis.
Complications of psoriasis can extend beyond the skin. Individuals with psoriasis are at an increased risk for comorbid conditions, including cardiovascular disease, metabolic syndrome, diabetes, and depression. The systemic inflammation associated with psoriasis is believed to contribute to these health issues, emphasizing the need for a holistic approach to treatment.
Diagnosis of Psoriasis
Clinical Evaluation
Diagnosing psoriasis typically begins with a thorough clinical evaluation by a dermatologist. The physician will assess the patient's medical history, family history, and the appearance of the skin lesions. A physical examination is conducted to identify the type of psoriasis and its severity.
In some cases, a skin biopsy may be performed to rule out other skin conditions and confirm the diagnosis. The biopsy involves taking a small sample of skin tissue for microscopic examination, which can reveal the characteristic features of psoriasis, such as hyperkeratosis and inflammatory infiltrates.
Diagnostic Tools
In addition to clinical evaluation, various diagnostic tools and questionnaires may be utilized to assess the impact of psoriasis on the patient's quality of life. The Psoriasis Area and Severity Index (PASI) is a commonly used scoring system that evaluates the severity of psoriasis based on the extent of body surface area affected and the severity of lesions. Other tools, such as the Dermatology Life Quality Index (DLQI), help gauge the psychosocial impact of the disease.
Treatment Options for Psoriasis
Topical Therapies
Topical treatments are often the first line of defense for mild to moderate psoriasis. These treatments are applied directly to the affected skin and include:
- Corticosteroids: Anti-inflammatory medications that help reduce redness and itching.
- Vitamin D Analogues: Such as calcipotriene, which slow down skin cell growth.
- Retinoids: Vitamin A derivatives that help normalize skin cell production.
- Coal Tar: A traditional treatment that helps reduce scaling and itching.
While topical therapies can be effective, they may not be sufficient for more severe cases, necessitating the use of systemic treatments.
Systemic Therapies
Systemic treatments target the entire body and are typically reserved for moderate to severe psoriasis or cases that do not respond to topical therapies. These include:
- Oral Medications: Such as methotrexate, cyclosporine, and acitretin, which suppress the immune system and reduce inflammation.
- Biologic Therapies: Targeted therapies that block specific pathways in the immune system. Examples include TNF-alpha inhibitors (e.g., etanercept, adalimumab) and IL-17 inhibitors (e.g., secukinumab).
While systemic therapies can be highly effective, they also carry risks of side effects and require careful monitoring by healthcare professionals.
Psychosocial Impact of Psoriasis
Emotional and Mental Health
The psychosocial impact of psoriasis can be profound. Many individuals with psoriasis experience feelings of embarrassment, anxiety, and depression due to the visible nature of their condition. The stigma associated with skin diseases can lead to social withdrawal and decreased quality of life.
Studies have shown that individuals with psoriasis are at a higher risk of developing comorbid mental health conditions, including depression and anxiety disorders. The chronic nature of the disease, coupled with its unpredictable flare-ups, can exacerbate these feelings, highlighting the importance of addressing mental health in the management of psoriasis.
Support and Resources
Support groups and educational resources can play a vital role in helping individuals cope with the emotional challenges of living with psoriasis. Organizations such as the National Psoriasis Foundation provide valuable information, support networks, and advocacy for those affected by the disease. Engaging with others who share similar experiences can foster a sense of community and reduce feelings of isolation.
Conclusion
Psoriasis is a complex and multifaceted condition that requires a comprehensive understanding of its pathophysiology, clinical manifestations, and treatment options. As research continues to evolve, new therapies and management strategies are emerging, offering hope to those affected by this chronic skin disorder. A holistic approach that considers both the physical and emotional aspects of psoriasis is essential for improving the quality of life for individuals living with this condition.
By fostering awareness, understanding, and compassion, we can create a supportive environment for those battling psoriasis, empowering them to seek the care and resources they need to manage their condition effectively.
Visit Our Offices
Services:
- • Medical Dermatology
- • Surgical Dermatology
- • Laser Treatments
- • Cosmetic Dermatology
Services:
- • Medical Dermatology
- • Surgical Dermatology
- • Laser Treatments
- • Cosmetic Dermatology
Visit Our Offices
Services:
- • Medical Dermatology
- • Surgical Dermatology
- • Laser Treatments
- • Cosmetic Dermatology
Services:
- • Medical Dermatology
- • Surgical Dermatology
- • Laser Treatments
- • Cosmetic Dermatology