Introduction to Warts
Warts are benign (non-cancerous) growths on the skin caused by the human papillomavirus (HPV). They can appear anywhere on the body but are most commonly found on the hands, feet, and face. Warts are characterized by their rough texture and can vary in size, shape, and color. They are typically harmless but can be bothersome due to their appearance or location.
The HPV virus that causes warts is highly contagious and can be transmitted through direct skin-to-skin contact or indirectly through contaminated surfaces. There are over 100 different types of HPV, and not all of them cause warts. Some strains are associated with more serious health issues, including certain types of cancer. Understanding the nature of warts and their causes is essential for effective treatment and prevention.
Warts can be classified into several categories, including common warts, plantar warts, flat warts, and genital warts. Each type has distinct characteristics and may require different approaches to treatment. The immune system plays a crucial role in the development and resolution of warts, as some individuals may be more susceptible to HPV infections than others.
Types of Warts
Common Warts
Common warts, also known as verrucae vulgaris, are typically found on the fingers, hands, and elbows. They are characterized by a rough, raised surface and can vary in color from skin-toned to brown or gray. Common warts are often mistaken for calluses or corns due to their texture, but they can be distinguished by the presence of tiny black dots, which are small blood vessels that have clotted.
These warts are usually harmless and may resolve on their own over time, but they can be persistent and may require treatment if they cause discomfort or embarrassment. Common warts are most prevalent in children and adolescents, likely due to their developing immune systems and increased exposure to HPV.
Plantar Warts
Plantar warts are found on the soles of the feet and are often flat due to the pressure of walking. They can be painful, especially when located on weight-bearing areas. Plantar warts may appear as small, rough bumps with a hardened surface and may also have black dots, similar to common warts. They can be mistaken for corns or calluses, but they are caused by HPV and require different treatment approaches.
The discomfort associated with plantar warts can lead individuals to seek treatment, as they can interfere with daily activities. Plantar warts are more common in individuals who walk barefoot in communal areas, such as swimming pools and locker rooms, where the virus can thrive in warm, moist environments.
Flat Warts
Flat warts, or verrucae planae, are smaller and smoother than common warts and can appear in clusters. They are often found on the face, neck, and arms and are more common in children and young adults. Flat warts are typically light brown, yellow, or pink and can be itchy or irritating. They may be more noticeable in individuals with darker skin tones due to their color contrast.
Flat warts may resolve on their own but can also persist for months or years. Treatment options are available for those who wish to remove them for cosmetic reasons or due to irritation. The choice of treatment depends on the individual's skin type, the number of warts, and their location.
Genital Warts
Genital warts are caused by specific strains of HPV and are considered a sexually transmitted infection (STI). They appear as small, flesh-colored or gray growths in the genital area, including the vulva, vagina, cervix, penis, and anus. Genital warts can be flat or raised and may occur in clusters, resembling a cauliflower-like appearance.
Unlike other types of warts, genital warts can have significant implications for sexual health, as they are associated with an increased risk of cervical cancer in women and other cancers in both men and women. Vaccination against HPV is available and recommended to prevent the development of genital warts and related cancers. Treatment for genital warts may include topical medications, cryotherapy, or surgical removal.
Diagnosis of Warts
Diagnosing warts typically involves a physical examination by a dermatologist or healthcare provider. The provider will assess the appearance, texture, and location of the growths to determine whether they are warts or another skin condition. In some cases, a biopsy may be performed to rule out other skin disorders or to confirm the diagnosis.
It is essential for individuals to seek medical advice if they notice changes in the appearance of their warts, such as changes in color, size, or shape, or if they experience pain or discomfort. These changes may indicate a need for further evaluation to rule out more serious conditions.
Treatment Options for Warts
Over-the-Counter Treatments
Over-the-counter (OTC) treatments for warts typically contain salicylic acid, which helps to exfoliate the wart and promote its removal. These treatments are available in various forms, including gels, pads, and liquids. Patients are advised to follow the instructions carefully and to be consistent with the application for optimal results.
While OTC treatments can be effective for common and plantar warts, they may take several weeks or months to achieve complete removal. It is essential to note that these treatments may not be suitable for all types of warts, particularly genital warts, which require specific medical interventions.
Prescription Treatments
For warts that do not respond to OTC treatments, healthcare providers may prescribe stronger topical medications, such as imiquimod or fluorouracil. These medications work by stimulating the immune system to fight the HPV virus or by inhibiting the growth of the wart tissue. Patients should discuss the potential side effects and benefits of these treatments with their healthcare provider.
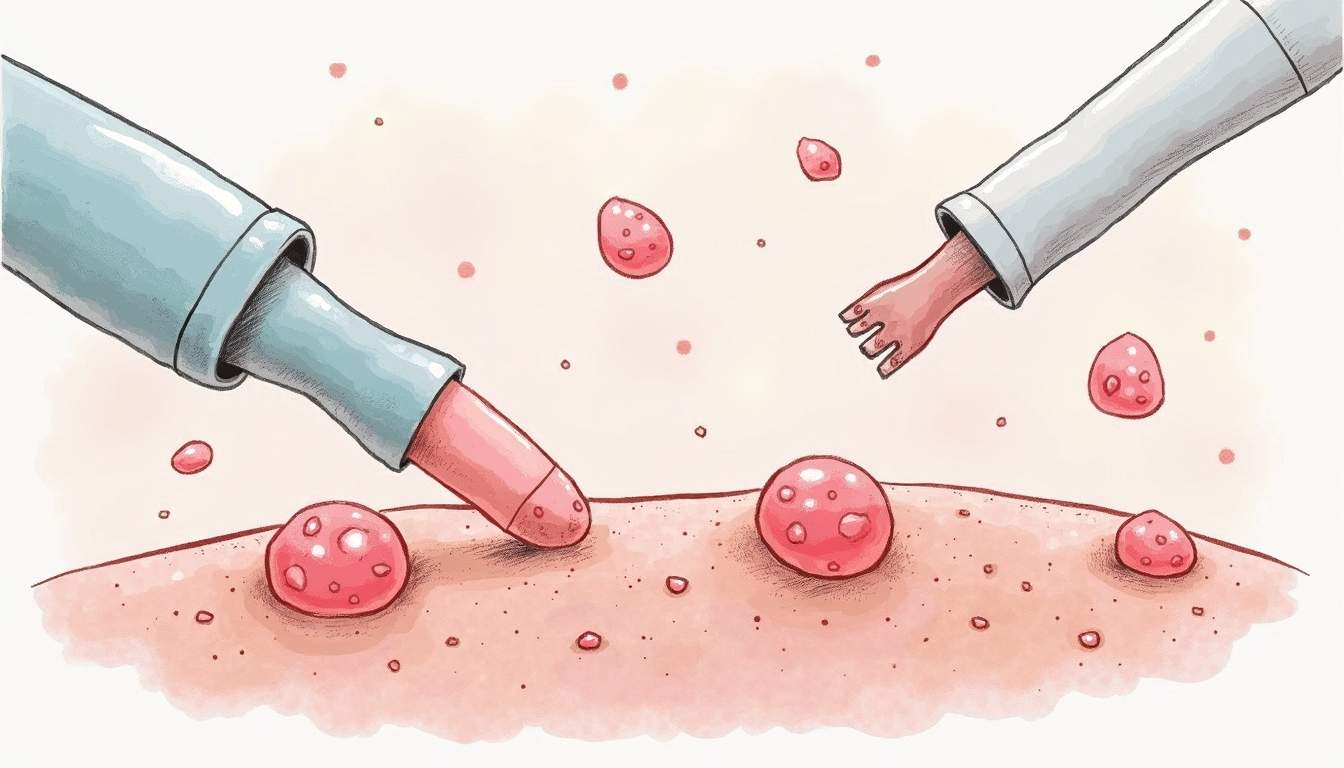
In some cases, a healthcare provider may recommend cryotherapy, which involves freezing the wart with liquid nitrogen. This method causes the wart to blister and eventually fall off. Cryotherapy is often effective for common and plantar warts and may require multiple sessions for complete removal.
Surgical Options
Surgical options for wart removal may be considered for stubborn warts that do not respond to other treatments. These procedures can include excision, where the wart is cut out, or electrosurgery, which uses electrical currents to destroy the wart tissue. Laser therapy is another option that can be effective for certain types of warts, particularly those that are difficult to treat.
Surgical removal may be performed in a dermatologist's office and typically requires local anesthesia. Patients should be aware of the potential for scarring and the need for aftercare following the procedure to promote healing and prevent infection.
Prevention of Warts
Preventing warts involves minimizing exposure to the HPV virus. Individuals can take several steps to reduce their risk of developing warts, including practicing good hygiene, avoiding direct contact with warts, and not sharing personal items such as towels or razors. Wearing flip-flops in communal areas, such as swimming pools and locker rooms, can also help prevent plantar warts.
Vaccination against HPV is a crucial preventive measure, particularly for adolescents and young adults. The HPV vaccine can significantly reduce the risk of developing genital warts and certain types of cancer associated with HPV. It is recommended for both males and females and is most effective when administered before the onset of sexual activity.
Conclusion
Warts are a common dermatological condition caused by the human papillomavirus, with various types requiring different treatment approaches. While most warts are benign and may resolve on their own, individuals seeking treatment should consult with a healthcare provider to determine the most appropriate options based on the type and location of the warts. Understanding the nature of warts, their causes, and prevention strategies can empower individuals to manage their skin health effectively.
With advancements in dermatological treatments and preventive measures, individuals can take proactive steps to address warts and reduce their risk of recurrence. Whether through over-the-counter treatments, prescription medications, or surgical interventions, effective options are available for those affected by warts. Education and awareness are key components in the fight against HPV and its associated conditions.
Visit Our Offices
Services:
- • Medical Dermatology
- • Surgical Dermatology
- • Laser Treatments
- • Cosmetic Dermatology
Services:
- • Medical Dermatology
- • Surgical Dermatology
- • Laser Treatments
- • Cosmetic Dermatology
Visit Our Offices
Services:
- • Medical Dermatology
- • Surgical Dermatology
- • Laser Treatments
- • Cosmetic Dermatology
Services:
- • Medical Dermatology
- • Surgical Dermatology
- • Laser Treatments
- • Cosmetic Dermatology