Introduction to Transplant Rejection
Transplant rejection is a complex immunological response that occurs when a recipient's immune system identifies transplanted tissue or organs as foreign. This phenomenon is particularly significant in dermatology, where skin grafts and transplants are common treatments for various conditions, including burns, skin cancers, and congenital defects. Understanding the mechanisms of transplant rejection is crucial for dermatologists, as it directly influences patient outcomes and the success of dermatological procedures.
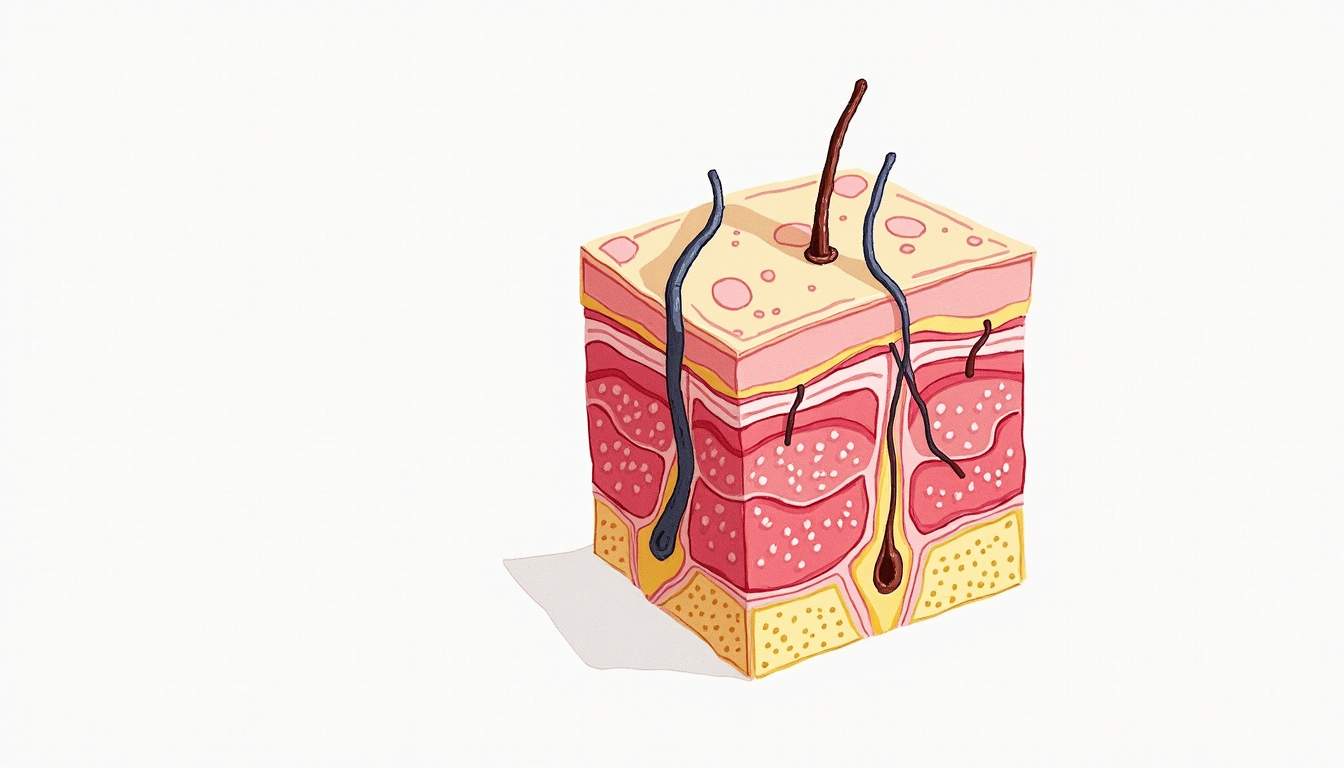
The skin is the largest organ of the body and serves as a critical barrier against environmental pathogens. When skin is transplanted, whether from a donor or the patient’s own body (in the case of autografts), the immune system may react to the foreign antigens present in the transplanted tissue. This reaction can lead to acute or chronic rejection, which can severely impact the viability of the graft and the overall health of the patient.
In this glossary entry, we will explore the various types of transplant rejection, the underlying immunological mechanisms, the clinical manifestations in dermatology, and the strategies employed to prevent and manage rejection in skin transplants.
Types of Transplant Rejection
Acute Rejection
Acute rejection is characterized by a rapid immune response that typically occurs within days to weeks following transplantation. This type of rejection is primarily mediated by T lymphocytes, which recognize foreign antigens on the surface of donor cells. Acute rejection can be further classified into two categories: cellular rejection and humoral rejection.
Cellular rejection involves the activation of CD4+ and CD8+ T cells, which attack the transplanted tissue. This process is often accompanied by the infiltration of immune cells into the graft, leading to inflammation and tissue damage. Clinically, acute cellular rejection may present with symptoms such as redness, swelling, and tenderness at the transplant site.
Humoral rejection, on the other hand, is mediated by antibodies produced against the donor’s antigens. This type of rejection can occur even in the absence of prior sensitization to the donor tissue. The presence of donor-specific antibodies can lead to complement activation and subsequent damage to the graft. In dermatology, humoral rejection may manifest as blistering or necrosis of the skin graft.
Chronic Rejection
Chronic rejection is a long-term process that can occur months to years after transplantation. It is characterized by a gradual decline in graft function and is often associated with chronic inflammation and fibrosis. The exact mechanisms underlying chronic rejection are not fully understood, but it is believed to involve a combination of immune-mediated injury and non-immune factors, such as ischemia and mechanical stress on the graft.
In dermatology, chronic rejection can lead to changes in the appearance and texture of the skin graft. Clinically, patients may experience symptoms such as thinning of the skin, loss of hair follicles, and the development of atrophic scars. Chronic rejection can significantly impact the aesthetic outcomes of skin grafts, making it a critical concern for dermatologists.
Immunological Mechanisms of Rejection
Cell-Mediated Immunity
Cell-mediated immunity plays a pivotal role in transplant rejection. T cells, particularly CD4+ helper T cells and CD8+ cytotoxic T cells, are central to the immune response against transplanted tissues. Upon recognition of foreign antigens presented by major histocompatibility complex (MHC) molecules on donor cells, T cells become activated and proliferate.
Activated CD4+ T cells release cytokines that recruit and activate other immune cells, including B cells and macrophages. CD8+ T cells directly attack and destroy donor cells, leading to graft damage. This process is often exacerbated by the presence of professional antigen-presenting cells (APCs) that enhance T cell activation and promote a robust immune response.
Humoral Immunity
Humoral immunity involves the production of antibodies by B cells in response to foreign antigens. In the context of transplant rejection, B cells can become activated by T cell help or through direct recognition of donor antigens. Once activated, B cells differentiate into plasma cells, which secrete antibodies that target the donor tissue.
These antibodies can bind to antigens on the surface of donor cells, leading to complement activation and the formation of membrane attack complexes that disrupt cell integrity. Additionally, the binding of antibodies can facilitate opsonization, marking donor cells for destruction by phagocytic immune cells. The role of humoral immunity in transplant rejection highlights the importance of monitoring antibody levels in patients undergoing skin transplantation.
Clinical Manifestations of Transplant Rejection in Dermatology
Signs and Symptoms
The clinical manifestations of transplant rejection in dermatology can vary widely depending on the type and severity of the rejection. In acute rejection, patients may present with localized erythema, swelling, and tenderness at the graft site. These symptoms are often accompanied by pain and discomfort, which can significantly affect the patient's quality of life.
In cases of humoral rejection, the skin graft may develop blisters, necrosis, or even complete loss of the grafted tissue. Chronic rejection, on the other hand, may present with more subtle changes, such as thinning of the skin, atrophy, and the development of fibrotic scars. These changes can lead to functional impairments and aesthetic concerns, necessitating further intervention from dermatologists.
Diagnostic Approaches
Diagnosing transplant rejection involves a combination of clinical evaluation, histopathological examination, and laboratory tests. Dermatologists often perform a thorough physical examination of the graft site, looking for signs of inflammation, necrosis, or other abnormalities. Skin biopsies may be taken to assess the histological features of rejection, including the presence of inflammatory infiltrates and tissue damage.
Additionally, laboratory tests may be conducted to measure the levels of donor-specific antibodies in the patient's serum. These tests can provide valuable information regarding the risk of humoral rejection and guide therapeutic decisions. Monitoring for signs of rejection is a critical component of post-transplant care, as early detection can significantly improve outcomes.
Prevention and Management of Transplant Rejection
Immunosuppressive Therapy
The cornerstone of preventing transplant rejection is the use of immunosuppressive therapy. These medications are designed to suppress the immune response and reduce the likelihood of rejection. Commonly used immunosuppressants include corticosteroids, calcineurin inhibitors (such as tacrolimus and cyclosporine), and antimetabolites (such as azathioprine and mycophenolate mofetil).
Immunosuppressive therapy is typically initiated immediately following transplantation and may be adjusted based on the patient's response and the occurrence of any adverse effects. While these medications are effective in preventing acute rejection, they also increase the risk of infections and malignancies, necessitating careful monitoring and management by dermatologists and other healthcare providers.
Monitoring and Follow-Up
Regular monitoring and follow-up are essential components of post-transplant care. Dermatologists play a crucial role in assessing the graft site for signs of rejection and managing any complications that may arise. Patients are often advised to maintain regular appointments for skin examinations, laboratory tests, and adjustments to their immunosuppressive regimen.
Education is also a vital aspect of follow-up care. Patients should be informed about the signs and symptoms of rejection and the importance of adhering to their medication regimen. Empowering patients with knowledge can lead to early detection of rejection and improved outcomes.
Conclusion
Transplant rejection is a multifaceted process that poses significant challenges in dermatology, particularly in the context of skin grafts and transplants. Understanding the types of rejection, the underlying immunological mechanisms, and the clinical manifestations is essential for dermatologists in providing optimal care for their patients.
Through the use of immunosuppressive therapy, vigilant monitoring, and patient education, dermatologists can effectively manage transplant rejection and improve the success rates of skin transplantation. As research continues to advance our understanding of transplant immunology, new strategies and therapies may emerge, further enhancing the field of dermatology and patient care.
Visit Our Offices
Services:
- • Medical Dermatology
- • Surgical Dermatology
- • Laser Treatments
- • Cosmetic Dermatology
Services:
- • Medical Dermatology
- • Surgical Dermatology
- • Laser Treatments
- • Cosmetic Dermatology
Visit Our Offices
Services:
- • Medical Dermatology
- • Surgical Dermatology
- • Laser Treatments
- • Cosmetic Dermatology
Services:
- • Medical Dermatology
- • Surgical Dermatology
- • Laser Treatments
- • Cosmetic Dermatology