Introduction to Scleroderma
Scleroderma, also known as systemic sclerosis, is a complex autoimmune disease characterized by the hardening and tightening of the skin and connective tissues. This condition can affect not only the skin but also internal organs, leading to significant health complications. The term "scleroderma" comes from the Greek words "sclero," meaning hard, and "derma," meaning skin. The disease is classified into two main types: localized scleroderma and systemic scleroderma, each presenting with distinct symptoms and implications for treatment.
Localized scleroderma primarily affects the skin and is often less severe than its systemic counterpart. It manifests in forms such as morphea and linear scleroderma. Systemic scleroderma, on the other hand, can affect multiple organ systems, including the lungs, heart, kidneys, and gastrointestinal tract, leading to a wide array of symptoms and complications. Understanding the pathology, symptoms, and treatment options for scleroderma is crucial for effective management and improving the quality of life for affected individuals.
Types of Scleroderma
Localized Scleroderma
Localized scleroderma is primarily confined to the skin and underlying tissues. It is generally less severe than systemic scleroderma and does not typically involve internal organs. The most common forms of localized scleroderma include:
- Morphea: Characterized by patches of hardened skin that can vary in size and color, often appearing as oval or circular lesions.
- Linear Scleroderma: This form presents as a line or band of hardened skin, often affecting the limbs or forehead, and can lead to growth disturbances in children.
Localized scleroderma can cause cosmetic concerns and discomfort, but it generally has a better prognosis compared to systemic scleroderma. Treatment often focuses on managing symptoms and may include topical therapies, physical therapy, and monitoring for any potential progression.
Systemic Scleroderma
Systemic scleroderma is a more severe form of the disease that can affect various internal organs, leading to significant health complications. It is further divided into two subtypes:
- Limited Scleroderma: Often referred to as CREST syndrome, it is characterized by Calcinosis, Raynaud's phenomenon, Esophageal dysfunction, Sclerodactyly, and Telangiectasia. Patients typically experience skin changes primarily on the face and hands, with a slower progression of internal organ involvement.
- Diffuse Scleroderma: This subtype is characterized by widespread skin involvement and a rapid onset of symptoms. It often leads to early and severe internal organ complications, including pulmonary fibrosis and renal crisis.
Systemic scleroderma can significantly impact a patient's quality of life, requiring a multidisciplinary approach to management, including rheumatologists, dermatologists, and other specialists.
Etiology and Pathophysiology
The exact cause of scleroderma remains unclear, but it is believed to involve a combination of genetic predisposition, environmental factors, and immune system dysregulation. Research indicates that certain genetic markers may increase susceptibility to the disease, while environmental triggers such as silica dust exposure, certain viral infections, and even specific medications may play a role in its onset.
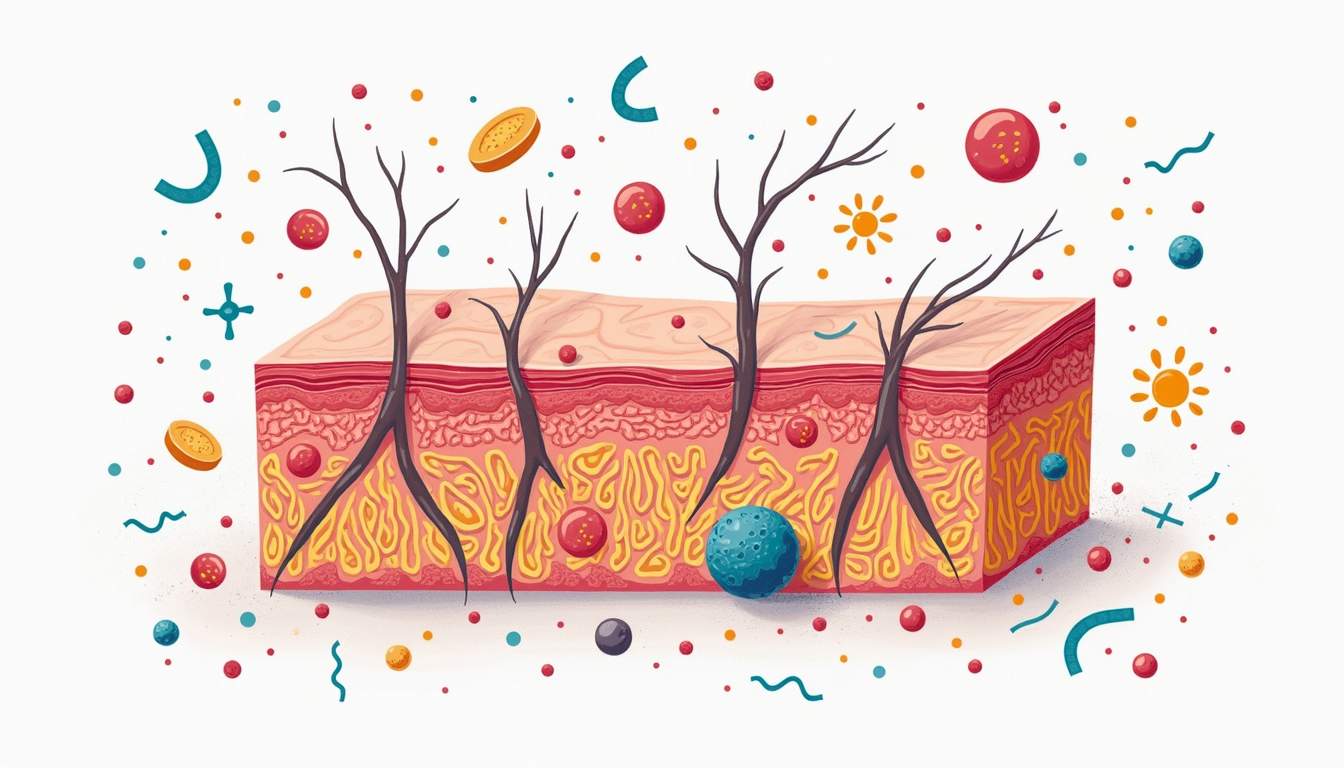
At the cellular level, scleroderma is characterized by an abnormal accumulation of collagen and other extracellular matrix components, leading to fibrosis or scarring of the skin and internal organs. This process is driven by an overactive immune response, where immune cells mistakenly attack healthy tissues, resulting in inflammation and subsequent fibrosis. The vascular system is also affected, with changes in blood vessel structure and function contributing to symptoms such as Raynaud's phenomenon, where blood flow to extremities is reduced in response to cold or stress.
Symptoms of Scleroderma
The symptoms of scleroderma can vary widely depending on the type and severity of the disease. Common symptoms include:
- Skin Changes: Thickening and hardening of the skin, often starting in the fingers and spreading to other areas. Skin may appear shiny and tight.
- Raynaud's Phenomenon: A condition where fingers and toes turn white or blue in response to cold or stress, due to reduced blood flow.
- Digestive Issues: Difficulty swallowing, acid reflux, and changes in bowel habits due to gastrointestinal involvement.
- Joint Pain: Arthritis or joint pain may occur, particularly in the hands and fingers.
- Fatigue: Many patients report chronic fatigue, which can significantly impact daily activities.
In cases of systemic scleroderma, additional symptoms may arise, including pulmonary hypertension, kidney dysfunction, and heart complications. The diverse range of symptoms necessitates a comprehensive evaluation by healthcare professionals to tailor an appropriate treatment plan.
Diagnosis of Scleroderma
Diagnosing scleroderma can be challenging due to its varied presentation and overlap with other autoimmune diseases. A thorough clinical evaluation is essential, including a detailed medical history and physical examination. Dermatologists often look for characteristic skin changes, while rheumatologists may assess for systemic involvement.
Diagnostic tests may include:
- Blood Tests: Tests for specific autoantibodies, such as anti-Scl-70 (topoisomerase I) and anti-centromere antibodies, can help confirm the diagnosis and determine the subtype of scleroderma.
- Skin Biopsy: A small sample of skin may be taken for histological examination to assess for fibrosis and other changes.
- Imaging Studies: X-rays, CT scans, or echocardiograms may be utilized to evaluate internal organ involvement, particularly the lungs and heart.
Early diagnosis is crucial for effective management and can significantly improve outcomes for patients with scleroderma.
Treatment Options for Scleroderma
There is currently no cure for scleroderma; however, treatment focuses on managing symptoms and preventing complications. A multidisciplinary approach is often employed, involving rheumatologists, dermatologists, physical therapists, and other specialists. Treatment options may include:
Medications
Medications play a vital role in managing scleroderma symptoms and preventing complications. Commonly prescribed medications include:
- Corticosteroids: These anti-inflammatory drugs can help reduce skin inflammation and improve symptoms.
- Immunosuppressants: Medications such as methotrexate and mycophenolate mofetil may be used to suppress the overactive immune response.
- Proton Pump Inhibitors: These are often prescribed to manage gastrointestinal symptoms, particularly acid reflux.
- Antihypertensives: Medications like calcium channel blockers can help manage Raynaud's phenomenon and pulmonary hypertension.
Physical Therapy
Physical therapy is an essential component of scleroderma management, particularly for patients experiencing joint stiffness and mobility issues. A physical therapist can develop a tailored exercise program to improve flexibility, strength, and overall function. Occupational therapy may also be beneficial for patients struggling with daily activities due to skin changes or joint pain.
Supportive Care
Supportive care is crucial for enhancing the quality of life for individuals with scleroderma. This may include:
- Psychological Support: Counseling and support groups can help patients cope with the emotional challenges of living with a chronic illness.
- Skin Care: Moisturizers and topical treatments can help manage skin dryness and discomfort.
- Dietary Modifications: A balanced diet may help manage gastrointestinal symptoms and overall health.
Prognosis and Living with Scleroderma
The prognosis for individuals with scleroderma varies significantly based on the type of scleroderma, the extent of organ involvement, and the response to treatment. Localized scleroderma generally has a favorable prognosis, with many patients experiencing spontaneous improvement over time. In contrast, systemic scleroderma can lead to serious complications, particularly if internal organs are affected.
Living with scleroderma requires ongoing management and support. Patients are encouraged to maintain regular follow-ups with healthcare providers to monitor disease progression and adjust treatment as necessary. Lifestyle modifications, such as stress management, regular exercise, and a healthy diet, can also contribute to improved well-being.
Conclusion
Scleroderma is a multifaceted autoimmune disease that poses unique challenges for patients and healthcare providers alike. Understanding the types, symptoms, diagnosis, and treatment options is essential for effective management. Ongoing research continues to shed light on the underlying mechanisms of scleroderma, paving the way for potential new therapies and improved outcomes for those affected by this complex condition.
Visit Our Offices
Services:
- • Medical Dermatology
- • Surgical Dermatology
- • Laser Treatments
- • Cosmetic Dermatology
Services:
- • Medical Dermatology
- • Surgical Dermatology
- • Laser Treatments
- • Cosmetic Dermatology
Visit Our Offices
Services:
- • Medical Dermatology
- • Surgical Dermatology
- • Laser Treatments
- • Cosmetic Dermatology
Services:
- • Medical Dermatology
- • Surgical Dermatology
- • Laser Treatments
- • Cosmetic Dermatology