Introduction to Lichen Planus
Lichen Planus is a chronic inflammatory condition that primarily affects the skin and mucous membranes. It is characterized by the presence of flat, purple, itchy lesions that can appear on various parts of the body, including the wrists, ankles, and lower back. The etiology of Lichen Planus is not fully understood, but it is believed to involve an autoimmune response where the body's immune system mistakenly attacks its own skin cells. This condition can also manifest in the oral cavity, leading to painful sores and lesions that can significantly impact a person's quality of life.
The term "lichen" refers to a symbiotic relationship between fungi and algae, while "planus" is derived from Latin, meaning flat. This nomenclature reflects the appearance of the lesions, which are typically flat-topped and polygonal in shape. Lichen Planus can occur in individuals of any age, but it is most commonly diagnosed in middle-aged adults. The condition is not contagious, and its exact prevalence is difficult to determine, but it is estimated to affect approximately 1% of the population.
Pathophysiology of Lichen Planus
The pathophysiology of Lichen Planus involves a complex interplay of immune-mediated processes. It is thought that certain triggers, such as medications, infections, or stress, may provoke an abnormal immune response. This response leads to the activation of T-cells, which are a type of white blood cell that plays a crucial role in the immune system. These activated T-cells migrate to the skin and mucous membranes, where they attack the basal layer of the epidermis, resulting in inflammation and the characteristic lesions of Lichen Planus.
Histologically, Lichen Planus is characterized by a band-like infiltrate of lymphocytes at the dermal-epidermal junction. This infiltrate is accompanied by liquefactive degeneration of the basal cell layer and the presence of "sawtooth" appearance of the epidermis. These histological findings are crucial for dermatologists in diagnosing Lichen Planus, particularly when lesions are atypical or when they occur in less common sites.
Clinical Presentation
Skin Lesions
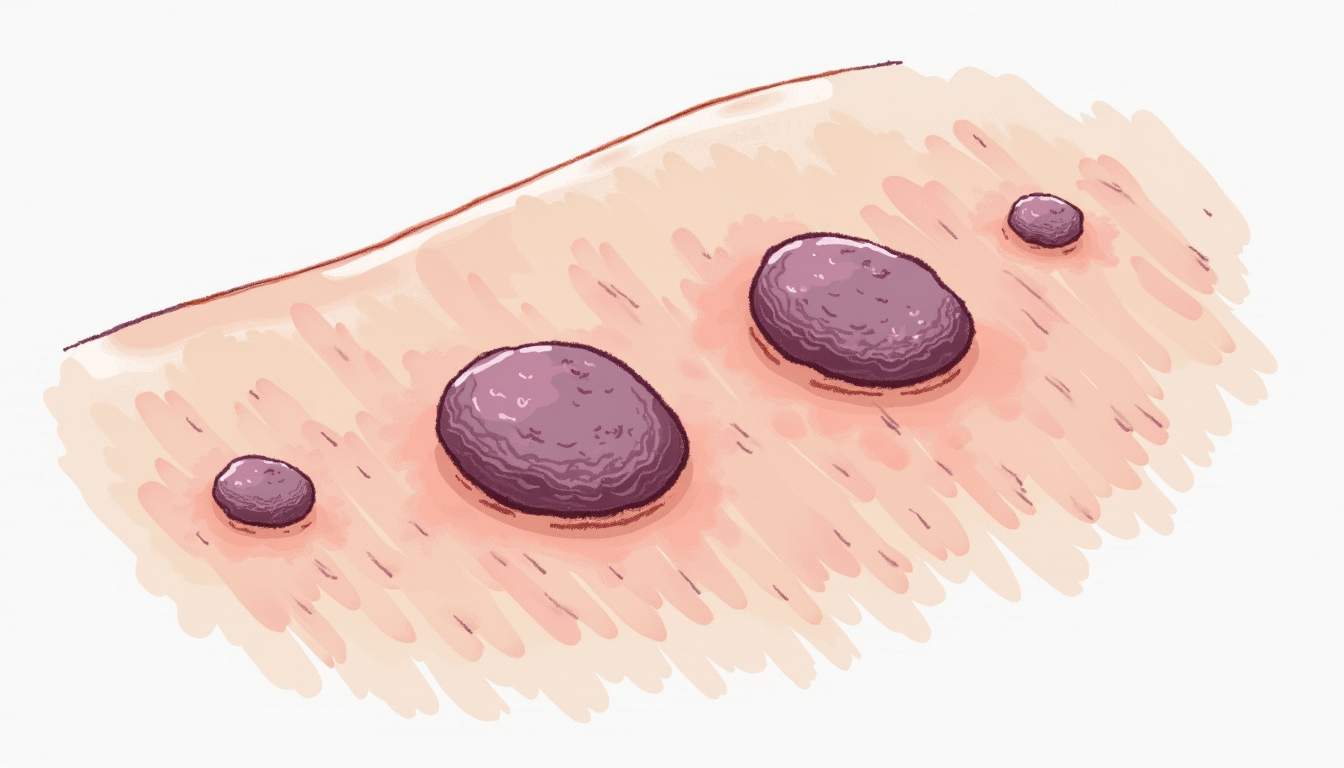
Skin lesions associated with Lichen Planus are typically flat-topped, polygonal papules that can vary in color from purple to reddish-brown. These lesions may be itchy and can appear in clusters or as individual spots. They are most commonly found on the flexor surfaces of the wrists, forearms, and ankles, but can also occur on the trunk, legs, and scalp. In some cases, the lesions may become hyperpigmented or hypopigmented after resolution, leading to post-inflammatory changes in skin color.
Oral Lichen Planus
Oral Lichen Planus is a common manifestation of the condition, affecting the mucous membranes of the mouth. It can present as white, lacy patches (known as Wickham's striae), painful ulcers, or erosive lesions that can cause significant discomfort during eating and speaking. Oral Lichen Planus can lead to complications such as secondary infections or, in rare cases, squamous cell carcinoma, necessitating careful monitoring and management.
Other Variants
In addition to classic Lichen Planus, there are several variants of the condition, including Lichen Planopilaris, which affects the hair follicles and can lead to hair loss, and Lichen Planus Pigmentosus, which is characterized by hyperpigmented macules, primarily in individuals with darker skin types. Each variant may have different clinical features and implications for treatment, highlighting the need for a thorough evaluation by a dermatologist.
Diagnosis of Lichen Planus
The diagnosis of Lichen Planus is primarily clinical, based on the characteristic appearance of the lesions and the patient's medical history. Dermatologists often perform a thorough physical examination to assess the distribution and morphology of the lesions. In cases where the diagnosis is uncertain, a skin biopsy may be performed to confirm the presence of the characteristic histological features associated with Lichen Planus.
Additional diagnostic tools, such as direct immunofluorescence, may be employed to differentiate Lichen Planus from other similar dermatoses, such as pemphigus or bullous pemphigoid. This technique involves the application of fluorescent antibodies to skin samples, allowing for the visualization of immune complex deposits that can aid in diagnosis.
Treatment Options
Topical Therapies
Topical corticosteroids are the first-line treatment for Lichen Planus, as they help to reduce inflammation and alleviate itching. These medications are applied directly to the affected areas and can be very effective in managing localized lesions. In cases where topical corticosteroids are insufficient, other topical agents such as calcineurin inhibitors (e.g., tacrolimus or pimecrolimus) may be used to help control symptoms.
Systemic Treatments
For more extensive or resistant cases of Lichen Planus, systemic treatments may be necessary. These can include oral corticosteroids, which can provide rapid relief of symptoms but are associated with potential side effects, especially with long-term use. Other systemic agents, such as retinoids, immunosuppressants (e.g., azathioprine or methotrexate), or biologic therapies, may be considered based on the severity of the disease and the patient's overall health.
Phototherapy
Phototherapy, particularly narrowband ultraviolet B (NB-UVB) therapy, has shown promise in treating Lichen Planus. This treatment involves exposing the skin to specific wavelengths of light, which can help reduce inflammation and promote healing. Phototherapy is typically reserved for cases that do not respond to topical or systemic treatments and requires careful monitoring to minimize the risk of skin damage.
Prognosis and Management
The prognosis for individuals with Lichen Planus varies, with many experiencing spontaneous resolution of lesions over time. However, the condition can be chronic and relapsing, necessitating ongoing management and follow-up with a dermatologist. Patients are encouraged to maintain regular appointments to monitor for any changes in their condition and to address any new symptoms that may arise.
In addition to medical management, lifestyle modifications can play a significant role in managing Lichen Planus. Patients are advised to avoid known triggers, such as certain medications, stress, and irritants, which may exacerbate their symptoms. Support groups and counseling may also be beneficial for individuals coping with the psychological impact of living with a chronic skin condition.
Conclusion
Lichen Planus is a multifaceted dermatological condition that requires a comprehensive understanding of its clinical presentation, pathophysiology, and treatment options. With appropriate management, many individuals can achieve significant improvement in their symptoms and quality of life. Ongoing research into the underlying mechanisms and potential therapeutic advancements holds promise for better outcomes in the future. Dermatologists play a crucial role in diagnosing and managing this condition, ensuring that patients receive the best possible care tailored to their individual needs.
Further Reading and Resources
For those seeking more information about Lichen Planus and related dermatological conditions, the following resources may be helpful:
Visit Our Offices
Services:
- • Medical Dermatology
- • Surgical Dermatology
- • Laser Treatments
- • Cosmetic Dermatology
Services:
- • Medical Dermatology
- • Surgical Dermatology
- • Laser Treatments
- • Cosmetic Dermatology
Visit Our Offices
Services:
- • Medical Dermatology
- • Surgical Dermatology
- • Laser Treatments
- • Cosmetic Dermatology
Services:
- • Medical Dermatology
- • Surgical Dermatology
- • Laser Treatments
- • Cosmetic Dermatology