Introduction to Tinea
Tinea, commonly referred to as ringworm, is a fungal infection that affects the skin, hair, and nails. Despite its name, tinea is not caused by a worm but rather by a group of fungi known as dermatophytes. These fungi thrive in warm, moist environments and can be found in various settings, including public showers, swimming pools, and locker rooms. Understanding tinea is essential for effective diagnosis and treatment, as well as for preventing its spread.
The term "tinea" is derived from the Latin word for "worm," which reflects the characteristic ring-like appearance of the rash that often accompanies the infection. Tinea can manifest in several forms, depending on the area of the body affected, and is classified into specific types based on its location.
In dermatology, tinea is a significant concern due to its contagious nature and the potential for misdiagnosis. It is crucial for both healthcare professionals and the general public to recognize the symptoms and understand the various types of tinea to ensure prompt and effective treatment.
Types of Tinea
Tinea is categorized based on the specific area of the body it affects. Each type has distinct characteristics and symptoms. The most common types of tinea include:
Tinea Corporis (Ringworm of the Body)
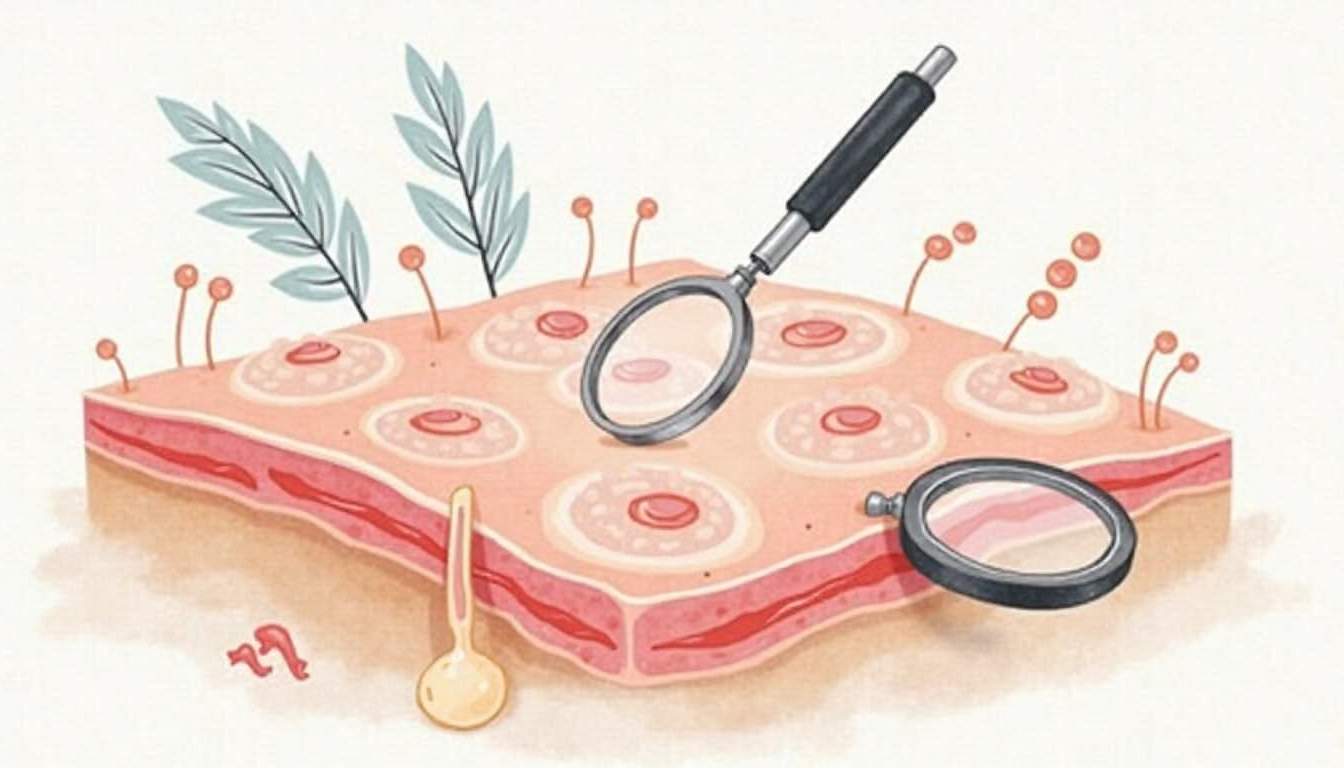
Tinea corporis is a fungal infection that affects the skin on the body, typically presenting as round, red patches with raised edges and a clear center. The lesions may be itchy and can spread if left untreated. This type of tinea is highly contagious and can be transmitted through direct contact with an infected person or by sharing contaminated items such as clothing, towels, or bedding.
Diagnosis is usually made through a physical examination, but in some cases, a skin scraping may be necessary to confirm the presence of dermatophytes. Treatment typically involves topical antifungal medications, although more severe cases may require oral antifungal therapy.
Tinea Pedis (Athlete's Foot)
Tinea pedis, commonly known as athlete's foot, is a fungal infection that primarily affects the feet, particularly the spaces between the toes. Symptoms include itching, burning, and peeling skin, which can lead to secondary bacterial infections if not treated. Tinea pedis is often associated with damp environments, such as locker rooms and swimming pools, where the fungi can thrive.
Prevention strategies include keeping the feet dry, wearing breathable footwear, and avoiding walking barefoot in communal areas. Treatment usually involves topical antifungal creams, powders, or sprays, and in more severe cases, oral antifungal medications may be prescribed.
Tinea Cruris (Jock Itch)
Tinea cruris, or jock itch, is a fungal infection that affects the groin area, inner thighs, and buttocks. It is characterized by a red, itchy rash that may have a well-defined border. This condition is more common in males and can be exacerbated by sweating and friction from clothing.
Diagnosis is typically made through clinical evaluation, and treatment involves the use of antifungal creams or powders. Maintaining good hygiene and keeping the area dry are crucial for preventing recurrence.
Tinea Capitis (Scalp Ringworm)
Tinea capitis is a fungal infection of the scalp that primarily affects children. It can cause hair loss, scaling, and inflammation. The infection may present as black dots (broken hair shafts) or as larger, scaly patches. Tinea capitis is often transmitted through direct contact with an infected person or animal, as well as through contaminated objects.
Diagnosis may require a fungal culture or microscopic examination of hair samples. Treatment typically involves oral antifungal medications, as topical treatments are often ineffective for this type of tinea. It is also essential to educate parents and caregivers about the importance of hygiene and avoiding sharing personal items to prevent the spread of the infection.
Causes and Risk Factors
Tinea infections are caused by dermatophytes, which are a group of fungi that require keratin for growth. These fungi can invade the outer layers of the skin, hair, and nails, leading to infection. Several factors can increase the risk of developing tinea, including:
- Moisture: Fungi thrive in warm, moist environments. Areas of the body that are frequently damp, such as the feet and groin, are particularly susceptible.
- Close Contact: Tinea is highly contagious and can spread through direct skin-to-skin contact or by sharing contaminated items such as towels, clothing, or sports equipment.
- Weakened Immune System: Individuals with compromised immune systems, such as those with diabetes or HIV/AIDS, are at a higher risk for developing tinea infections.
- Poor Hygiene: Inadequate personal hygiene can contribute to the development and spread of tinea infections.
Symptoms and Diagnosis
The symptoms of tinea can vary depending on the type of infection and the area of the body affected. Common symptoms include:
- Itching: This is often the first symptom and can range from mild to severe.
- Red, Scaly Patches: These may have raised edges and a clear center, giving them a ring-like appearance.
- Hair Loss: In cases of tinea capitis, hair may become brittle and fall out.
- Peeling Skin: This is particularly common in tinea pedis and tinea cruris.
Diagnosis of tinea is primarily based on clinical examination. However, laboratory tests may be performed to confirm the diagnosis. These tests can include:
- Skin Scraping: A sample of the affected skin may be taken and examined under a microscope for the presence of fungi.
- Fungal Culture: This involves growing the fungus in a laboratory setting to identify the specific type of dermatophyte causing the infection.
- Wood's Lamp Examination: Some types of fungi will fluoresce under ultraviolet light, aiding in diagnosis.
Treatment Options
Treatment for tinea infections typically involves antifungal medications, which can be administered topically or orally depending on the severity and location of the infection. The main classes of antifungal agents used include:
Topical Antifungals
Topical antifungal treatments are often the first line of defense for localized tinea infections. These medications are applied directly to the affected area and include:
- Clotrimazole: An over-the-counter antifungal cream effective against various dermatophytes.
- Miconazole: Another common topical antifungal that can be found in creams and powders.
- Terbinafine: A potent antifungal that is available in both topical and oral forms.
Oral Antifungals
In cases of widespread infection or tinea capitis, oral antifungal medications may be necessary. These include:
- Griseofulvin: Often used for tinea capitis, it works by inhibiting fungal cell division.
- Fluconazole: A broad-spectrum antifungal that can be effective against various types of fungi.
- Itraconazole: Another oral antifungal that is used for more severe or resistant infections.
Prevention Strategies
Preventing tinea infections involves a combination of good hygiene practices and lifestyle changes. Some effective strategies include:
- Keep Skin Dry: Moisture encourages fungal growth, so it is essential to dry areas prone to sweating, such as the feet and groin.
- Avoid Sharing Personal Items: Do not share towels, clothing, or sports equipment to reduce the risk of transmission.
- Wear Breathable Clothing: Choose loose-fitting, breathable fabrics to minimize moisture buildup on the skin.
- Practice Good Hygiene: Regular bathing and changing into clean clothes can help prevent fungal infections.
Conclusion
Tinea is a common dermatological condition that can affect individuals of all ages. Understanding its types, causes, symptoms, and treatment options is crucial for effective management and prevention. By practicing good hygiene and being aware of the risk factors, individuals can reduce their chances of developing tinea infections. If symptoms arise, seeking prompt medical attention is essential to ensure a proper diagnosis and appropriate treatment.
In summary, while tinea infections can be bothersome and uncomfortable, they are generally treatable with antifungal medications. Awareness and education about this condition can empower individuals to take proactive steps in maintaining their skin health and preventing the spread of infection.
Visit Our Offices
Services:
- • Medical Dermatology
- • Surgical Dermatology
- • Laser Treatments
- • Cosmetic Dermatology
Services:
- • Medical Dermatology
- • Surgical Dermatology
- • Laser Treatments
- • Cosmetic Dermatology
Visit Our Offices
Services:
- • Medical Dermatology
- • Surgical Dermatology
- • Laser Treatments
- • Cosmetic Dermatology
Services:
- • Medical Dermatology
- • Surgical Dermatology
- • Laser Treatments
- • Cosmetic Dermatology