Introduction to Skin Vascularity
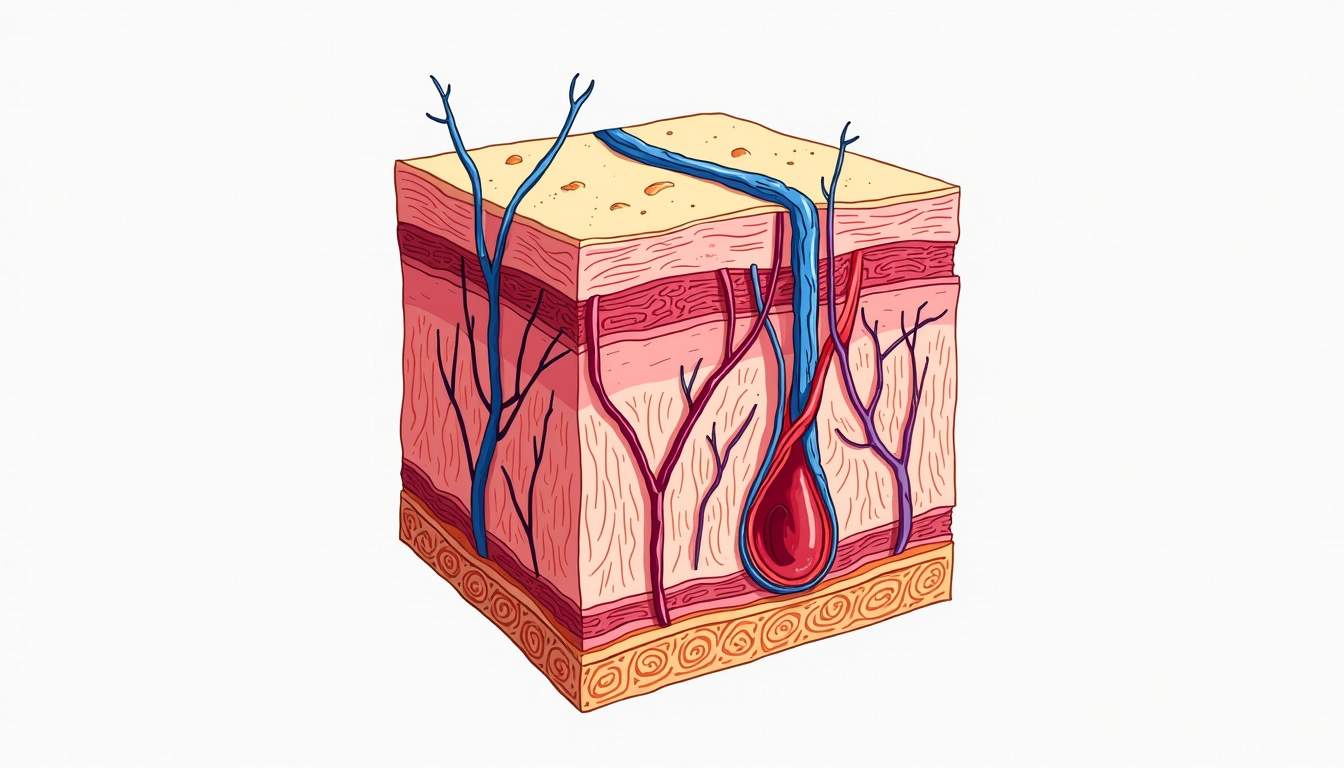
Skin vascularity refers to the distribution and density of blood vessels within the skin. This concept is crucial in dermatology as it plays a significant role in various physiological processes, including thermoregulation, nutrient delivery, and waste removal. Understanding skin vascularity is essential for diagnosing and treating various skin conditions, as well as for aesthetic procedures. The vascular system in the skin is composed of a complex network of arteries, veins, and capillaries, each serving a unique function.
The skin is the largest organ of the human body, and its vascular system is intricately designed to support its numerous functions. The vascularity of the skin can vary significantly between individuals and can be influenced by factors such as genetics, age, environmental factors, and overall health. In dermatology, assessing skin vascularity can provide insights into underlying health conditions, skin disorders, and the effectiveness of certain treatments.
Components of Skin Vascularity
Arteries
Arteries are blood vessels that carry oxygenated blood away from the heart to various tissues, including the skin. In the skin, the primary arteries include the superficial and deep dermal arteries. These arteries branch into smaller arterioles, which further divide into capillaries. The arterial supply is crucial for maintaining skin health, as it provides essential nutrients and oxygen to skin cells.
In dermatology, the assessment of arterial supply can help identify conditions such as ischemia, where insufficient blood flow can lead to skin necrosis or ulceration. Additionally, understanding arterial patterns can be beneficial during surgical procedures, such as skin grafting or excisions, to minimize complications and ensure adequate blood supply to the healing tissue.
Veins
Veins are responsible for returning deoxygenated blood back to the heart. In the skin, venous drainage occurs through a network of superficial and deep veins. Superficial veins are located just beneath the epidermis and are often visible, especially in individuals with fair skin or low body fat. Deep veins, on the other hand, are located deeper within the dermis and are less visible.
In dermatology, the evaluation of venous return is essential for diagnosing conditions such as chronic venous insufficiency, varicose veins, and venous ulcers. These conditions can lead to significant morbidity and may require interventions such as compression therapy or surgical procedures to improve venous flow and alleviate symptoms.
Capillaries
Capillaries are the smallest blood vessels and serve as the primary site for the exchange of gases, nutrients, and waste products between blood and tissues. The capillary network in the skin is extensive, allowing for efficient nutrient delivery and waste removal. Capillary density can vary based on skin type, location on the body, and individual health status.
In dermatology, capillary function is often assessed in conditions such as rosacea, where increased capillary permeability leads to redness and flushing. Additionally, capillary refill time is a quick clinical test used to assess peripheral circulation and can provide insights into overall vascular health.
Factors Affecting Skin Vascularity
Genetic Factors
Genetics play a significant role in determining an individual's skin vascularity. Certain genetic predispositions can lead to variations in the number and distribution of blood vessels in the skin. For instance, individuals with a family history of conditions such as rosacea or telangiectasia may be more likely to exhibit increased vascularity in the skin.
Moreover, genetic factors can influence skin thickness, elasticity, and overall health, which can indirectly affect vascularity. Understanding these genetic influences can help dermatologists tailor treatment plans for conditions associated with abnormal skin vascularity.
Environmental Factors
Environmental factors, including sun exposure, temperature, and pollution, can significantly impact skin vascularity. Prolonged sun exposure can lead to the development of abnormal blood vessels, such as actinic telangiectasia, which are often seen in sun-damaged skin. Additionally, extreme temperatures can cause vasodilation or vasoconstriction, affecting blood flow to the skin.
Pollution and other environmental stressors can also lead to inflammation and vascular changes in the skin. Dermatologists often consider these factors when diagnosing and treating skin conditions, as addressing environmental influences can be crucial for effective management.
Age and Hormonal Changes
As individuals age, the skin undergoes various changes, including alterations in vascularity. Aging skin tends to have a reduced vascular supply, which can contribute to a decrease in skin elasticity and an increased risk of skin injuries. Hormonal changes, particularly during puberty, pregnancy, and menopause, can also influence skin vascularity. For example, increased estrogen levels during pregnancy can lead to the development of spider veins and other vascular changes.
Understanding the impact of age and hormonal fluctuations on skin vascularity is essential for dermatologists, as it can guide treatment decisions and help manage age-related skin conditions effectively.
Clinical Significance of Skin Vascularity
Diagnosis of Skin Conditions
Skin vascularity is a critical factor in diagnosing various dermatological conditions. Conditions such as psoriasis, eczema, and dermatitis often present with changes in vascularity, including increased redness and swelling due to inflammation. Dermatologists utilize these vascular changes as diagnostic clues to differentiate between various skin disorders.
Moreover, conditions like skin cancer can also exhibit abnormal vascular patterns. For instance, the presence of atypical blood vessels in a mole may raise suspicion for melanoma. Therefore, a thorough understanding of skin vascularity is essential for accurate diagnosis and timely intervention.
Management of Vascular Disorders
In dermatology, managing vascular disorders often involves addressing underlying causes and symptoms. Treatments may include laser therapy, sclerotherapy, or topical medications aimed at reducing vascular lesions or improving circulation. Understanding the vascular anatomy of the skin is crucial for dermatologists when selecting appropriate treatment modalities.
Additionally, lifestyle modifications, such as weight management, regular exercise, and smoking cessation, can improve overall vascular health and reduce the risk of developing vascular-related skin conditions. Dermatologists often provide comprehensive care that includes education on these lifestyle changes to enhance treatment outcomes.
Aesthetic Considerations of Skin Vascularity
Cosmetic Procedures
Skin vascularity plays a significant role in aesthetic dermatology, particularly in procedures aimed at enhancing skin appearance. Treatments such as laser resurfacing, chemical peels, and microdermabrasion can affect vascularity and, consequently, skin tone and texture. Understanding the vascular response to these treatments is essential for achieving optimal results and minimizing complications.
Moreover, aesthetic procedures such as fillers and injectables may also influence vascularity. For instance, the injection of hyaluronic acid fillers can temporarily increase local vascularity, enhancing the overall appearance of the skin. Dermatologists must be skilled in managing these vascular changes to ensure patient safety and satisfaction.
Skin Rejuvenation
Rejuvenating the skin often involves addressing vascularity to improve overall skin health and appearance. Treatments aimed at reducing vascular lesions, such as laser therapy for rosacea or spider veins, can significantly enhance skin tone and texture. Additionally, promoting healthy blood flow through techniques such as microneedling can stimulate collagen production and improve skin vitality.
In summary, understanding skin vascularity is essential for both clinical and aesthetic dermatology. It provides valuable insights into skin health, guides treatment decisions, and enhances patient outcomes. Dermatologists must remain informed about the complexities of skin vascularity to provide comprehensive care and achieve optimal results for their patients.
Conclusion
Skin vascularity is a multifaceted aspect of dermatology that encompasses the intricate network of blood vessels within the skin. Its significance extends beyond mere anatomy, influencing various physiological processes, diagnostic evaluations, and treatment strategies. By understanding the components, factors affecting vascularity, and its clinical and aesthetic implications, dermatologists can provide comprehensive care that addresses both health and cosmetic concerns.
As research in dermatology continues to evolve, the understanding of skin vascularity will undoubtedly deepen, leading to more effective treatments and improved patient outcomes. Whether addressing skin conditions or enhancing aesthetic appearance, a thorough grasp of skin vascularity remains a cornerstone of dermatological practice.
Visit Our Offices
Services:
- • Medical Dermatology
- • Surgical Dermatology
- • Laser Treatments
- • Cosmetic Dermatology
Services:
- • Medical Dermatology
- • Surgical Dermatology
- • Laser Treatments
- • Cosmetic Dermatology
Visit Our Offices
Services:
- • Medical Dermatology
- • Surgical Dermatology
- • Laser Treatments
- • Cosmetic Dermatology
Services:
- • Medical Dermatology
- • Surgical Dermatology
- • Laser Treatments
- • Cosmetic Dermatology