Introduction to Skin Lesions
Skin lesions are abnormal changes in the skin's structure or appearance, which can arise from a variety of causes, including infections, inflammatory conditions, and neoplastic processes. They can manifest in numerous forms, such as rashes, bumps, or discolorations, and can be indicative of underlying health issues. Understanding skin lesions is crucial for both diagnosis and treatment in dermatology.
In dermatology, the term "skin lesion" encompasses a wide range of conditions, from benign growths to malignant tumors. Their classification is based on various factors, including morphology, etiology, and the underlying skin pathology. This comprehensive glossary aims to elucidate the different types of skin lesions, their characteristics, and their clinical significance.
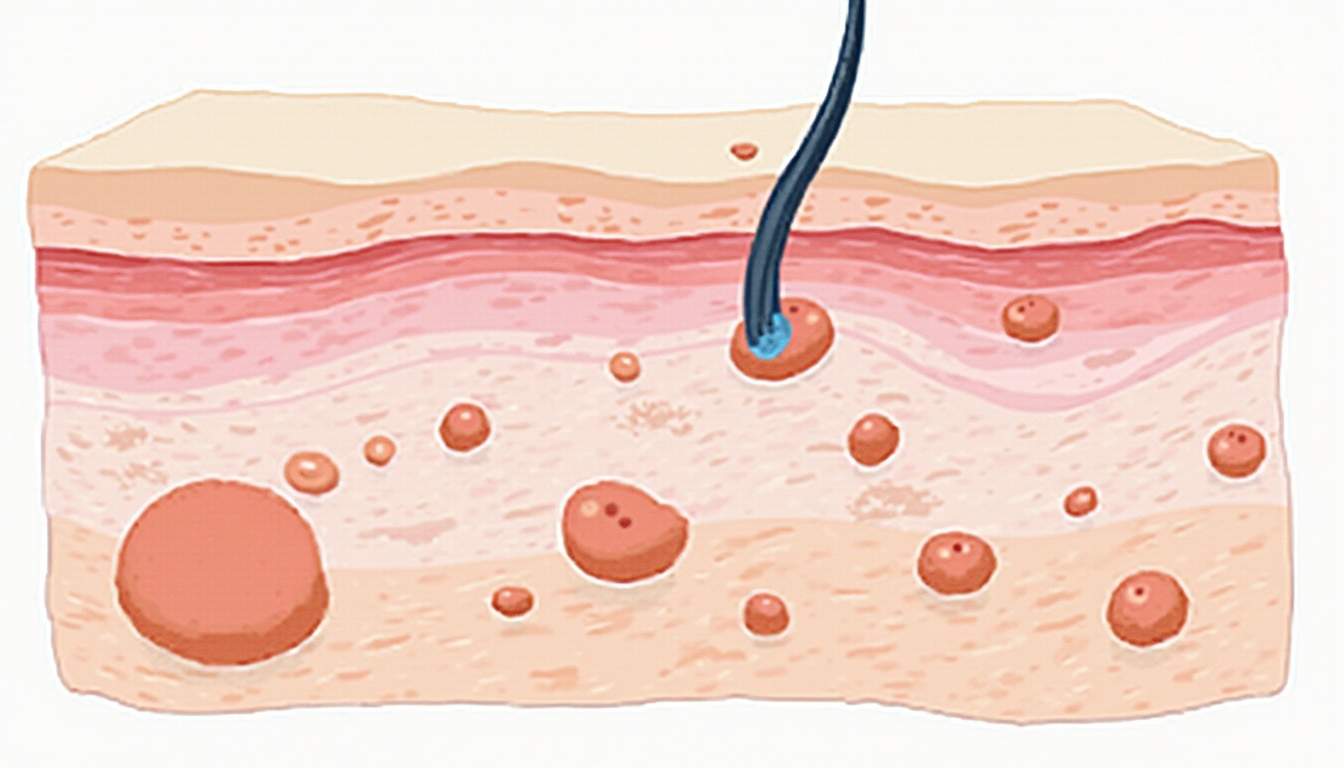
Skin lesions can be classified into primary and secondary lesions. Primary lesions are those that arise directly from a disease process, while secondary lesions are changes that occur as a result of primary lesions. This distinction is vital for dermatologists when assessing and diagnosing skin conditions.
Types of Skin Lesions
Primary Skin Lesions
Primary skin lesions are the initial manifestations of a disease and can be categorized into several types based on their appearance and characteristics. These include macules, papules, plaques, nodules, vesicles, pustules, and tumors. Each type has distinct features that aid in diagnosis.
1. Macules are flat, discolored areas of the skin that are less than 1 cm in diameter. They do not involve any change in texture or elevation. Common examples include freckles and flat moles.
2. Papules are small, raised bumps on the skin, typically less than 1 cm in diameter. They can be caused by various conditions, including acne, warts, and insect bites. Papules may be itchy or painful, depending on their underlying cause.
3. Plaques are larger, raised areas of skin that are often formed by the confluence of multiple papules. They can be scaly and are commonly seen in conditions like psoriasis.
4. Nodules are solid, raised lesions that are larger than papules, often extending deeper into the skin. They can be caused by infections, cysts, or tumors.
5. Vesicles are small, fluid-filled blisters that are less than 1 cm in diameter, often seen in conditions like herpes simplex virus infections.
6. Pustules are similar to vesicles but contain pus. They are commonly associated with acne and other inflammatory skin conditions.
7. Skin tumors can be benign or malignant growths that arise from various skin cells. They require careful evaluation to determine their nature and appropriate management.
Secondary Skin Lesions
Secondary skin lesions develop as a consequence of primary lesions or due to external factors such as scratching or infection. They include scales, crusts, excoriations, fissures, ulcers, and scars. Understanding these lesions is essential for effective treatment and management.
1. Scales are flakes of dead skin that can be dry or oily. They are often associated with conditions like eczema or psoriasis, where the skin's natural shedding process is disrupted.
2. Crusts form when dried serum, blood, or pus accumulates on the skin's surface, often resulting from a rupture of vesicles or pustules. They are commonly seen in impetigo.
3. Excoriations are linear abrasions caused by scratching the skin. They can lead to secondary infections if not managed properly.
4. Fissures are linear splits in the skin, often occurring in areas of thickened skin, such as the palms or soles, and can be quite painful.
5. Ulcers are deeper losses of skin integrity that can result from various causes, including pressure, infection, or systemic diseases.
6. Scars are fibrous tissues that replace normal skin after injury or surgery. They can vary in appearance and texture, depending on the healing process.
Common Causes of Skin Lesions
Skin lesions can arise from a multitude of factors, including infectious agents, autoimmune diseases, environmental exposures, and genetic predispositions. Understanding these causes is essential for effective diagnosis and treatment.
1. Infections are a common cause of skin lesions. Bacterial infections, such as impetigo or cellulitis, can lead to pustules and crusting. Viral infections, such as herpes simplex or varicella-zoster, can cause vesicular lesions. Fungal infections, like tinea, can lead to scaling and erythema.
2. Autoimmune diseases can also manifest as skin lesions. Conditions like lupus erythematosus and psoriasis are characterized by inflammatory lesions that can significantly impact the quality of life.
3. Environmental factors, such as sun exposure, can lead to lesions like actinic keratosis or skin cancer. Chemical irritants and allergens can also cause contact dermatitis, resulting in rashes and lesions.
4. Genetic predispositions play a significant role in the development of certain skin lesions. Conditions like neurofibromatosis and familial melanoma syndromes highlight the importance of genetic factors in dermatological health.
Diagnosis of Skin Lesions
The diagnosis of skin lesions involves a comprehensive assessment that includes a detailed medical history, physical examination, and sometimes additional diagnostic tests. Dermatologists utilize various techniques to accurately identify the nature of skin lesions.
1. Medical history is crucial in understanding the context of skin lesions. Patients are often asked about the onset, duration, and progression of the lesions, as well as any associated symptoms such as itching, pain, or discharge.
2. Physical examination involves a thorough inspection of the skin, where dermatologists assess the size, shape, color, and texture of the lesions. They may also examine the surrounding skin for any signs of inflammation or infection.
3. Diagnostic tests may be necessary for a definitive diagnosis. These can include skin biopsies, where a small sample of skin is removed for histopathological examination, and cultures to identify infectious agents. Dermatoscopy, a non-invasive imaging technique, can also aid in the evaluation of pigmented lesions.
Treatment Options for Skin Lesions
Treatment for skin lesions varies widely depending on the underlying cause, type of lesion, and patient factors. Options range from topical therapies to surgical interventions, and the choice of treatment is guided by the specific diagnosis.
1. Topical therapies are often the first line of treatment for many skin lesions. Corticosteroids, retinoids, and antifungal creams can effectively manage inflammatory and infectious lesions.
2. Systemic medications may be necessary for more severe cases, particularly in autoimmune conditions. Immunosuppressants and biologic agents are commonly used in conditions like psoriasis and lupus.
3. Surgical interventions may be required for the removal of malignant lesions or to excise large benign tumors. Techniques such as cryotherapy, electrosurgery, and laser therapy are also utilized for various skin lesions.
4. Patient education is a critical component of treatment. Dermatologists often provide guidance on skin care practices, sun protection, and lifestyle modifications to prevent recurrence and promote skin health.
Prevention of Skin Lesions
Preventing skin lesions involves a combination of protective measures, lifestyle choices, and regular dermatological care. While not all skin lesions can be prevented, certain strategies can significantly reduce the risk.
1. Sun protection is paramount in preventing skin lesions, particularly skin cancers. Using broad-spectrum sunscreen, wearing protective clothing, and avoiding peak sun exposure can help mitigate UV damage.
2. Skin care routines that include gentle cleansing and moisturizing can help maintain skin integrity and prevent conditions like eczema and dermatitis.
3. Avoiding irritants and allergens is crucial for individuals prone to contact dermatitis. Identifying and avoiding triggers can significantly reduce the incidence of skin lesions.
4. Regular dermatological check-ups are essential for early detection and management of skin lesions, particularly for individuals with a history of skin cancer or other risk factors.
Conclusion
Skin lesions are a diverse and complex topic within dermatology, encompassing a wide range of conditions that can significantly impact an individual's health and quality of life. Understanding the various types of skin lesions, their causes, diagnostic approaches, treatment options, and preventive measures is essential for effective management.
As dermatological science continues to evolve, ongoing research and advancements in technology will further enhance our understanding and treatment of skin lesions. Patients are encouraged to seek professional advice for any concerning skin changes and to engage in proactive skin care practices.
In summary, skin lesions are not merely cosmetic concerns; they can be indicative of underlying health issues that require attention. By fostering awareness and understanding, we can improve outcomes and promote better skin health for all.
Visit Our Offices
Services:
- • Medical Dermatology
- • Surgical Dermatology
- • Laser Treatments
- • Cosmetic Dermatology
Services:
- • Medical Dermatology
- • Surgical Dermatology
- • Laser Treatments
- • Cosmetic Dermatology
Visit Our Offices
Services:
- • Medical Dermatology
- • Surgical Dermatology
- • Laser Treatments
- • Cosmetic Dermatology
Services:
- • Medical Dermatology
- • Surgical Dermatology
- • Laser Treatments
- • Cosmetic Dermatology