Introduction to Seborrheic Dermatitis
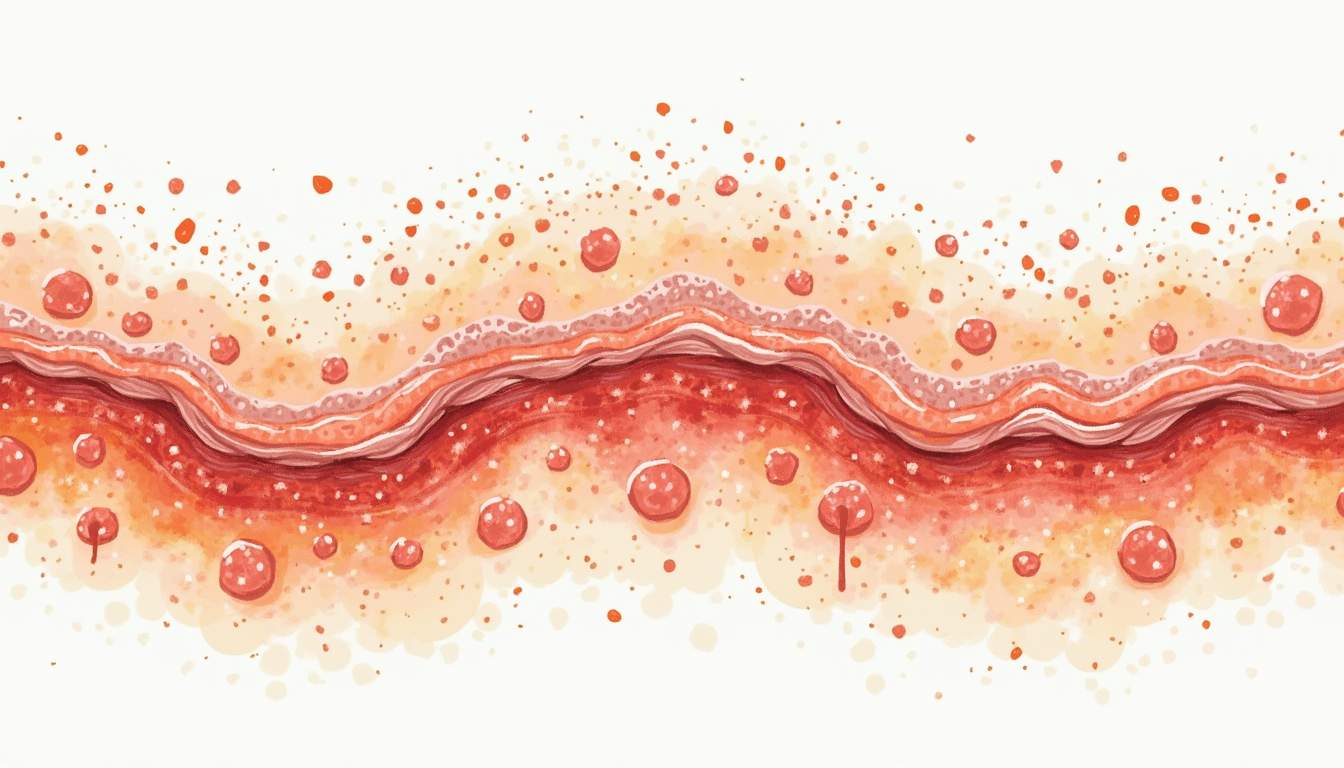
Seborrheic dermatitis is a common, chronic inflammatory skin condition characterized by red, flaky, greasy patches of skin. It primarily affects areas of the body that are rich in sebaceous (oil) glands, such as the scalp, face, and upper back. This condition is often confused with other skin disorders, making accurate diagnosis and treatment essential for effective management.
The exact cause of seborrheic dermatitis remains unclear, but it is believed to be multifactorial, involving a combination of genetic, environmental, and microbial factors. The condition is often exacerbated by stress, hormonal changes, and certain weather conditions, particularly cold and dry climates. Understanding the underlying mechanisms of seborrheic dermatitis can help in developing effective treatment strategies.
In this glossary entry, we will explore the various aspects of seborrheic dermatitis, including its symptoms, causes, risk factors, diagnosis, treatment options, and preventive measures. This comprehensive overview aims to provide a thorough understanding of the condition for both patients and healthcare professionals.
Symptoms of Seborrheic Dermatitis
The symptoms of seborrheic dermatitis can vary widely among individuals and may range from mild to severe. Common symptoms include:
- Red, inflamed skin: The affected areas often appear red and irritated, which can be particularly noticeable on lighter skin tones.
- Flaky or scaly patches: These patches may be white or yellowish in color and can appear greasy or dry, depending on the severity of the condition.
- Itching and discomfort: Many individuals experience itching, which can lead to scratching and further irritation of the skin.
- Crusty lesions: In some cases, especially in infants, seborrheic dermatitis can lead to the formation of crusty lesions, commonly referred to as cradle cap.
Symptoms can fluctuate, often improving during warmer months and worsening during colder, drier seasons. In infants, seborrheic dermatitis is typically self-limiting and may resolve on its own within a few months, while in adults, it may persist for years and require ongoing management.
Causes of Seborrheic Dermatitis
The precise cause of seborrheic dermatitis is not fully understood, but several factors are believed to contribute to its development. These include:
- Malassezia yeast: This fungus is a normal inhabitant of the skin but may overgrow in certain individuals, leading to inflammation and the characteristic symptoms of seborrheic dermatitis.
- Sebum production: An increase in sebum production can create an environment conducive to fungal overgrowth, exacerbating the condition.
- Genetic predisposition: A family history of seborrheic dermatitis or other skin conditions may increase the likelihood of developing this disorder.
- Immune system response: An abnormal immune response to the Malassezia fungus may trigger inflammation and the symptoms associated with seborrheic dermatitis.
Additionally, certain medical conditions, such as Parkinson's disease, HIV/AIDS, and other immunocompromising conditions, have been linked to an increased risk of seborrheic dermatitis. Stress and hormonal fluctuations may also play a role in exacerbating symptoms, highlighting the complex interplay of factors involved in this condition.
Risk Factors for Seborrheic Dermatitis
Several risk factors can increase the likelihood of developing seborrheic dermatitis. These include:
- Age: Seborrheic dermatitis can occur at any age but is most commonly seen in infants and adults aged 30 to 60 years.
- Skin type: Individuals with oily skin are more prone to developing seborrheic dermatitis due to increased sebum production.
- Weather conditions: Cold, dry weather can exacerbate symptoms, while warm, humid conditions may provide some relief.
- Stress: High levels of stress can trigger or worsen symptoms, making stress management an important aspect of treatment.
Understanding these risk factors can help individuals identify their susceptibility to seborrheic dermatitis and take proactive measures to manage their skin health effectively.
Diagnosis of Seborrheic Dermatitis
Diagnosing seborrheic dermatitis typically involves a thorough clinical evaluation by a dermatologist. The process may include:
- Medical history: The dermatologist will inquire about the patient's medical history, including any previous skin conditions, family history, and current symptoms.
- Physical examination: A detailed examination of the affected areas will be conducted to assess the appearance and distribution of the lesions.
- Exclusion of other conditions: The dermatologist may perform tests to rule out other skin disorders that may present similarly, such as psoriasis, eczema, or contact dermatitis.
In most cases, seborrheic dermatitis can be diagnosed based on clinical findings alone. However, in atypical cases or when secondary infections are suspected, additional tests such as skin scrapings or biopsies may be performed to confirm the diagnosis and guide treatment.
Treatment Options for Seborrheic Dermatitis
Treatment for seborrheic dermatitis aims to reduce inflammation, control symptoms, and prevent flare-ups. Various options are available, including:
- Topical treatments: These include medicated shampoos containing ingredients such as ketoconazole, selenium sulfide, or zinc pyrithione, which help to control fungal growth and reduce inflammation. Topical corticosteroids may also be prescribed to alleviate itching and redness.
- Oral medications: In more severe cases, systemic treatments such as oral antifungals or corticosteroids may be considered, particularly if topical therapies are ineffective.
- Phototherapy: Light therapy, including ultraviolet (UV) light exposure, may be beneficial for some individuals with extensive or resistant seborrheic dermatitis.
- Lifestyle modifications: Implementing a regular skincare routine, managing stress, and avoiding known triggers can significantly improve symptoms and reduce the frequency of flare-ups.
It is essential for individuals with seborrheic dermatitis to work closely with their healthcare provider to develop a personalized treatment plan that addresses their specific needs and concerns.
Preventive Measures for Seborrheic Dermatitis
While seborrheic dermatitis may not be entirely preventable, several strategies can help minimize the risk of flare-ups and manage symptoms effectively:
- Regular cleansing: Gently cleansing the affected areas with mild, non-irritating cleansers can help remove excess oil and flakes, reducing the likelihood of flare-ups.
- Moisturization: Using non-comedogenic moisturizers can help maintain skin hydration and barrier function, which is essential for managing seborrheic dermatitis.
- Avoiding irritants: Identifying and avoiding products that may irritate the skin, such as harsh soaps, fragrances, and alcohol-based products, can help prevent exacerbation of symptoms.
- Stress management: Incorporating stress-reduction techniques, such as mindfulness, yoga, or regular exercise, can be beneficial in managing seborrheic dermatitis.
By adopting these preventive measures, individuals can take an active role in managing their seborrheic dermatitis and improving their overall skin health.
Conclusion
Seborrheic dermatitis is a prevalent skin condition that can significantly impact an individual's quality of life. Understanding its symptoms, causes, risk factors, diagnosis, treatment options, and preventive measures is crucial for effective management. By working closely with healthcare professionals and implementing appropriate strategies, individuals can successfully navigate the challenges posed by seborrheic dermatitis and maintain healthy skin.
As research continues to evolve, new insights into the underlying mechanisms and treatment options for seborrheic dermatitis may emerge, offering hope for improved management of this chronic condition. Staying informed and proactive is key to achieving optimal skin health and well-being.
Visit Our Offices
Services:
- • Medical Dermatology
- • Surgical Dermatology
- • Laser Treatments
- • Cosmetic Dermatology
Services:
- • Medical Dermatology
- • Surgical Dermatology
- • Laser Treatments
- • Cosmetic Dermatology
Visit Our Offices
Services:
- • Medical Dermatology
- • Surgical Dermatology
- • Laser Treatments
- • Cosmetic Dermatology
Services:
- • Medical Dermatology
- • Surgical Dermatology
- • Laser Treatments
- • Cosmetic Dermatology