Introduction to Psoriatic Arthritis
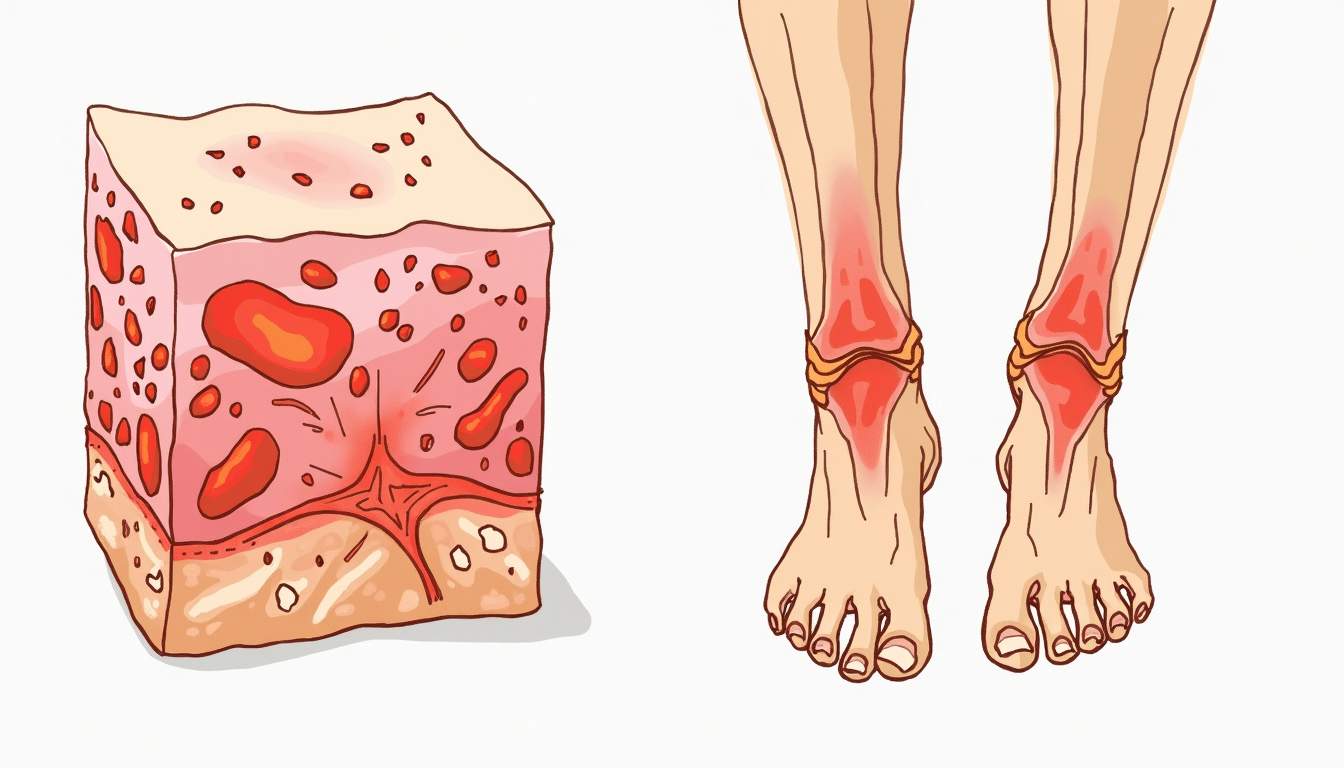
Psoriatic arthritis (PsA) is a chronic inflammatory condition that affects both the skin and joints. It is associated with psoriasis, a skin disorder characterized by red, scaly patches. PsA can lead to joint pain, stiffness, and swelling, and it can significantly impact the quality of life for those affected. Understanding the relationship between psoriasis and psoriatic arthritis is crucial for effective management and treatment.
The condition is classified as an autoimmune disorder, where the immune system mistakenly attacks healthy cells, leading to inflammation. PsA can manifest in various forms, and its symptoms can range from mild to severe. The prevalence of psoriatic arthritis is estimated to be around 30% among individuals with psoriasis, making it a significant concern in dermatology.
In this glossary entry, we will explore the various aspects of psoriatic arthritis, including its symptoms, causes, diagnosis, treatment options, and its relationship with dermatological conditions. This comprehensive overview aims to provide a thorough understanding of PsA for both patients and healthcare professionals.
Symptoms of Psoriatic Arthritis
The symptoms of psoriatic arthritis can vary widely among individuals, but they typically include joint pain, swelling, and stiffness. These symptoms can occur in any joint in the body, including the fingers, toes, wrists, knees, and spine. The severity of symptoms can fluctuate, with periods of exacerbation followed by periods of remission.
In addition to joint symptoms, many patients also experience skin manifestations associated with psoriasis. These can include:
- Plaques: Raised, red patches covered with silvery-white scales.
- Nail changes: Pitting, discoloration, and separation of the nail from the nail bed.
- Enthesitis: Inflammation at the sites where tendons and ligaments attach to bones, often causing pain in the heels or under the feet.
- Sacroiliitis: Inflammation of the sacroiliac joints, which can lead to lower back pain.
Fatigue is also a common complaint among individuals with psoriatic arthritis, which can be debilitating and affect daily activities. Recognizing these symptoms early is essential for timely diagnosis and treatment.
Causes and Risk Factors
The exact cause of psoriatic arthritis remains unclear, but it is believed to involve a combination of genetic, environmental, and immunological factors. Family history plays a significant role, as individuals with a family history of psoriasis or psoriatic arthritis are at a higher risk of developing the condition.
Environmental triggers can also contribute to the onset of psoriatic arthritis. These may include:
- Infections: Certain infections, particularly streptococcal throat infections, have been linked to the onset of psoriasis and PsA.
- Injury: Physical trauma to the skin or joints can trigger the development of psoriatic arthritis.
- Stress: Psychological stress may exacerbate symptoms and contribute to flare-ups.
- Obesity: Excess weight can increase the risk of developing psoriatic arthritis and worsen existing symptoms.
Understanding these risk factors can help individuals take proactive steps to manage their health and potentially reduce the likelihood of developing psoriatic arthritis.
Diagnosis of Psoriatic Arthritis
Diagnosing psoriatic arthritis can be challenging due to the overlap of symptoms with other forms of arthritis. A thorough medical history, physical examination, and diagnostic tests are essential for an accurate diagnosis. Healthcare providers typically assess the following:
- Medical History: A detailed history of symptoms, family history of psoriasis or arthritis, and any previous skin conditions.
- Physical Examination: A comprehensive examination of the joints, skin, and nails to identify signs of inflammation or psoriasis.
- Imaging Studies: X-rays or MRI scans may be used to assess joint damage or inflammation.
- Laboratory Tests: Blood tests may be conducted to rule out other forms of arthritis, such as rheumatoid arthritis, and to check for markers of inflammation.
Early diagnosis is crucial for effective management of psoriatic arthritis, as it can help prevent joint damage and improve long-term outcomes.
Treatment Options for Psoriatic Arthritis
Treatment for psoriatic arthritis aims to reduce inflammation, alleviate pain, and prevent joint damage. A multidisciplinary approach is often employed, involving dermatologists, rheumatologists, and primary care physicians. Treatment options may include:
- Nonsteroidal Anti-Inflammatory Drugs (NSAIDs): These medications help relieve pain and reduce inflammation.
- DMARDs (Disease-Modifying Antirheumatic Drugs): Medications such as methotrexate can slow the progression of the disease and prevent joint damage.
- Biologic Therapies: Targeted therapies that focus on specific components of the immune system, such as TNF inhibitors and IL-17 inhibitors, have shown promising results in managing PsA.
- Topical Treatments: For skin symptoms, topical corticosteroids and vitamin D analogs may be prescribed to manage psoriasis.
- Physical Therapy: Exercise and physical therapy can help improve joint function and reduce stiffness.
It is essential for patients to work closely with their healthcare providers to develop a personalized treatment plan that addresses their specific needs and preferences.
Living with Psoriatic Arthritis
Living with psoriatic arthritis can be challenging, as the condition can affect both physical and emotional well-being. Patients often experience fluctuations in symptoms, which can impact daily activities, work, and social interactions. It is important for individuals to adopt a holistic approach to managing their condition.
Strategies for coping with psoriatic arthritis may include:
- Education: Understanding the condition and its management options can empower patients to make informed decisions about their health.
- Support Networks: Connecting with support groups or communities can provide emotional support and shared experiences.
- Healthy Lifestyle Choices: Maintaining a balanced diet, engaging in regular physical activity, and managing stress can positively impact overall health and well-being.
- Regular Follow-Up: Consistent communication with healthcare providers is essential for monitoring the condition and adjusting treatment as needed.
By adopting these strategies, individuals with psoriatic arthritis can enhance their quality of life and better manage their symptoms.
Conclusion
Psoriatic arthritis is a complex condition that requires a comprehensive understanding of its symptoms, causes, diagnosis, and treatment options. As a dermatological concern, it highlights the intricate relationship between skin health and joint health. Early diagnosis and a tailored treatment approach are crucial for managing psoriatic arthritis effectively.
As research continues to evolve, new therapies and management strategies are being developed, offering hope for improved outcomes for individuals living with this condition. By staying informed and proactive, patients can navigate the challenges of psoriatic arthritis and lead fulfilling lives.
Visit Our Offices
Services:
- • Medical Dermatology
- • Surgical Dermatology
- • Laser Treatments
- • Cosmetic Dermatology
Services:
- • Medical Dermatology
- • Surgical Dermatology
- • Laser Treatments
- • Cosmetic Dermatology
Visit Our Offices
Services:
- • Medical Dermatology
- • Surgical Dermatology
- • Laser Treatments
- • Cosmetic Dermatology
Services:
- • Medical Dermatology
- • Surgical Dermatology
- • Laser Treatments
- • Cosmetic Dermatology