Definition of Pruritus
Pruritus, commonly referred to as itching, is a sensation that provokes the desire to scratch. This phenomenon can be localized to a specific area of the skin or can be generalized across the entire body. Itching is a complex sensory experience that can be triggered by a variety of factors, including but not limited to skin conditions, systemic diseases, and environmental irritants. Understanding pruritus is essential for dermatologists and healthcare providers as it can significantly impact a patient's quality of life.
The sensation of itch is mediated by a variety of pathways in the nervous system, primarily involving the activation of specific nerve fibers known as C-fibers. These fibers transmit signals to the central nervous system, where they are interpreted as the sensation of itching. This response can be influenced by numerous factors, including psychological states, which can exacerbate or alleviate the sensation of itch.
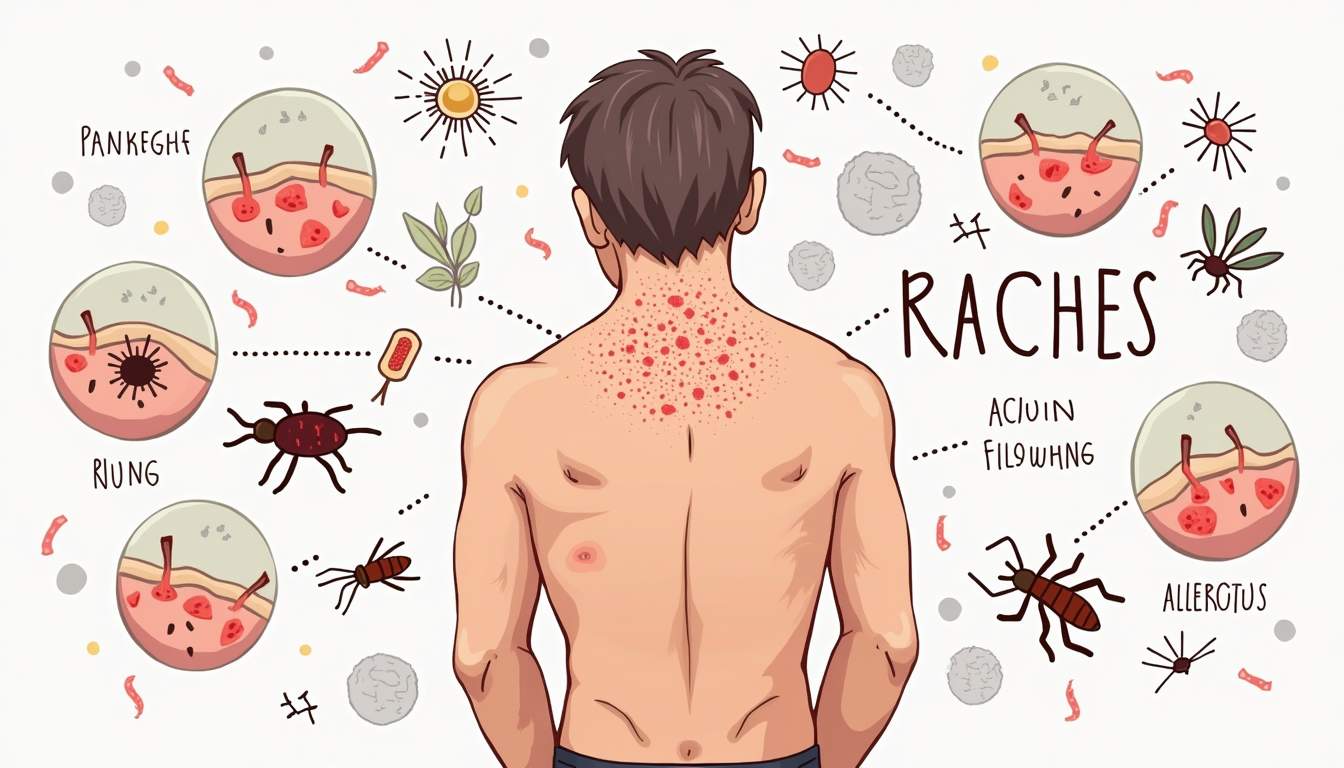
Pruritus can be classified into two main categories: acute and chronic. Acute pruritus lasts for a short duration, often associated with transient conditions such as insect bites or allergic reactions. Chronic pruritus, on the other hand, persists for six weeks or longer and is often linked to underlying medical conditions such as eczema, psoriasis, or liver disease. The distinction between acute and chronic pruritus is crucial for determining the appropriate diagnostic and therapeutic approaches.
Causes of Pruritus
The causes of pruritus are diverse and can be broadly categorized into dermatological, systemic, and psychological factors. Dermatological causes include a range of skin conditions such as eczema, psoriasis, contact dermatitis, and urticaria (hives). Each of these conditions has its own unique pathophysiology and treatment options, making it essential for healthcare providers to conduct thorough assessments to identify the underlying cause of the itching.
Systemic causes of pruritus can include liver disease, kidney failure, thyroid disorders, and certain malignancies. In these cases, the itch may not be confined to a specific area of the body and can be generalized. For instance, patients with liver disease may experience pruritus due to the accumulation of bile salts in the bloodstream, which can stimulate itch receptors. Similarly, chronic kidney disease can lead to pruritus as a result of uremic toxins affecting the skin and nervous system.
Psychological factors can also play a significant role in the experience of pruritus. Conditions such as anxiety, depression, and stress can exacerbate the sensation of itching, leading to a vicious cycle where the itch leads to scratching, which in turn causes further irritation and inflammation of the skin. Understanding the interplay between psychological and physical factors is essential for developing comprehensive treatment plans for patients suffering from chronic pruritus.
Types of Pruritus
Localized Pruritus
Localized pruritus refers to itching that is confined to a specific area of the body. This type of itch is often associated with dermatological conditions such as eczema, contact dermatitis, or insect bites. The localized nature of this itch can make it easier to diagnose and treat, as the underlying cause is often apparent based on the appearance of the skin and the patient's history.
Common examples of localized pruritus include the itch associated with poison ivy exposure, which is due to an allergic reaction to the plant's oil, urushiol. In such cases, topical treatments such as corticosteroids or antihistamines may be effective in alleviating the itch. Additionally, localized pruritus can occur in response to infections such as scabies or fungal infections, where the itch is often accompanied by other symptoms such as redness, swelling, or the presence of a rash.
Generalized Pruritus
Generalized pruritus, on the other hand, affects larger areas of the body and can be more challenging to diagnose. This type of itch is often associated with systemic conditions, such as liver disease or renal failure, where the underlying cause may not be immediately apparent. Patients may experience generalized itching without any visible skin lesions, making it essential for healthcare providers to conduct thorough evaluations, including laboratory tests and imaging studies, to identify the underlying cause.
In cases of generalized pruritus, treatment often focuses on addressing the underlying condition. For example, managing liver disease may involve medications to reduce bile salt accumulation, while renal failure may require dialysis. In addition to treating the underlying cause, symptomatic relief can be provided through the use of topical emollients, antihistamines, or systemic medications such as corticosteroids.
Diagnosis of Pruritus
The diagnosis of pruritus involves a comprehensive evaluation that includes a detailed medical history, physical examination, and, when necessary, laboratory tests. The healthcare provider will typically begin by asking the patient about the duration, location, and characteristics of the itch, as well as any associated symptoms such as rash, redness, or swelling. This information is crucial for narrowing down the potential causes of pruritus.
During the physical examination, the provider will assess the skin for any visible lesions, rashes, or signs of inflammation. The presence of specific skin findings can provide valuable clues regarding the underlying cause of the itch. For instance, the presence of scaly patches may suggest psoriasis, while vesicular lesions may indicate contact dermatitis or herpes simplex infection.
In some cases, laboratory tests may be necessary to identify systemic causes of pruritus. These tests may include blood tests to assess liver and kidney function, thyroid function tests, and skin biopsies to evaluate for specific dermatological conditions. A thorough diagnostic workup is essential for developing an effective treatment plan tailored to the individual patient's needs.
Treatment Options for Pruritus
Treatment for pruritus is highly individualized and depends on the underlying cause, the severity of symptoms, and the patient's overall health. In cases of localized pruritus, topical treatments are often the first line of defense. These may include corticosteroid creams, which can reduce inflammation and alleviate itching, or topical antihistamines that can block itch signals at the site of application.
For generalized pruritus, systemic treatments may be necessary. Antihistamines, particularly first-generation antihistamines such as diphenhydramine, can be effective in providing relief from itching, although they may cause sedation. In cases where pruritus is associated with systemic conditions, medications targeting the underlying disease may be required. For example, patients with chronic kidney disease may benefit from medications that reduce uremic toxins, while those with liver disease may require treatments to manage bile salt accumulation.
In addition to pharmacological treatments, non-pharmacological approaches can also be beneficial in managing pruritus. These may include lifestyle modifications such as avoiding known irritants, using gentle skin care products, and maintaining proper hydration of the skin through the use of emollients. Behavioral therapies, such as cognitive-behavioral therapy (CBT), can also be effective in addressing the psychological aspects of chronic pruritus, helping patients develop coping strategies to manage their symptoms.
Complications of Pruritus
While pruritus itself is a symptom, it can lead to significant complications if not properly managed. One of the most common complications is secondary skin infections resulting from scratching. When the skin barrier is compromised due to repeated scratching, it becomes more susceptible to bacterial or fungal infections, which can exacerbate the itching and lead to further complications.
In addition to skin infections, chronic pruritus can have a profound impact on a patient's quality of life. The constant urge to scratch can interfere with sleep, leading to insomnia and fatigue. This, in turn, can contribute to psychological issues such as anxiety and depression, creating a cycle of worsening symptoms. Patients may also experience social withdrawal or decreased productivity due to the discomfort associated with pruritus.
Addressing the complications of pruritus requires a comprehensive approach that includes both medical treatment and supportive care. Healthcare providers should work closely with patients to develop individualized management plans that address not only the physical symptoms of pruritus but also the psychological and social aspects of living with chronic itching.
Conclusion
Pruritus is a complex and multifaceted symptom that can arise from a wide range of causes, both dermatological and systemic. Understanding the underlying mechanisms, types, and treatment options for pruritus is essential for healthcare providers in order to effectively manage this condition and improve patient outcomes. Through a thorough diagnostic workup and a tailored treatment approach, it is possible to alleviate the discomfort associated with pruritus and enhance the overall quality of life for affected individuals.
As research continues to advance our understanding of pruritus, new therapeutic options and management strategies are likely to emerge, offering hope for patients suffering from this challenging symptom. Ongoing education and awareness among healthcare providers and patients alike will be crucial in addressing the complexities of pruritus and ensuring effective care for those affected.
Visit Our Offices
Services:
- • Medical Dermatology
- • Surgical Dermatology
- • Laser Treatments
- • Cosmetic Dermatology
Services:
- • Medical Dermatology
- • Surgical Dermatology
- • Laser Treatments
- • Cosmetic Dermatology
Visit Our Offices
Services:
- • Medical Dermatology
- • Surgical Dermatology
- • Laser Treatments
- • Cosmetic Dermatology
Services:
- • Medical Dermatology
- • Surgical Dermatology
- • Laser Treatments
- • Cosmetic Dermatology