Introduction to Pityriasis Versicolor
Pityriasis Versicolor, also known as Tinea Versicolor, is a common skin condition characterized by the presence of discolored patches on the skin. It is caused by an overgrowth of a type of yeast that is normally found on the skin, specifically Malassezia furfur. This condition is not contagious and primarily affects the outer layer of the skin, leading to a variety of pigmentation changes that can be both aesthetically concerning and symptomatic for some individuals.
The condition is particularly prevalent in warm, humid climates, where the yeast thrives. It can affect individuals of any age, but it is most commonly seen in adolescents and young adults. Understanding the underlying mechanisms, symptoms, and treatment options for Pityriasis Versicolor is crucial for effective management and prevention of recurrence.
This glossary entry aims to provide a comprehensive overview of Pityriasis Versicolor, including its etiology, clinical presentation, diagnosis, treatment options, and prevention strategies. By exploring these facets, individuals can gain a better understanding of this dermatological condition and how to address it effectively.
Etiology of Pityriasis Versicolor
Microbial Factors
The primary causative agent of Pityriasis Versicolor is the Malassezia yeast, which is a part of the normal flora of human skin. Under certain conditions, such as increased humidity, excessive sweating, or hormonal changes, this yeast can proliferate excessively, leading to the characteristic skin changes associated with the condition. The overgrowth of Malassezia leads to the production of dicarboxylic acids, which inhibit the enzyme tyrosinase, crucial for melanin production in the skin. This inhibition results in the hypopigmented or hyperpigmented lesions seen in affected individuals.
Other contributing factors include genetic predisposition, oily skin, and certain environmental conditions. Individuals with a family history of Pityriasis Versicolor may be more susceptible to developing the condition. Additionally, those with compromised immune systems or other skin conditions may also be at a higher risk due to their altered skin barrier function.
Environmental and Lifestyle Factors
Environmental factors play a significant role in the development of Pityriasis Versicolor. Warm, humid climates are particularly conducive to the growth of Malassezia yeast. Activities that promote sweating, such as exercise or exposure to heat, can exacerbate the condition. Furthermore, certain lifestyle choices, such as poor hygiene, excessive use of oily skin products, or wearing tight clothing, can create an environment that favors yeast overgrowth.
Dietary factors may also influence the condition. Some studies suggest that high sugar intake and diets low in certain nutrients may contribute to the proliferation of Malassezia. However, more research is needed to establish a definitive link between diet and Pityriasis Versicolor.
Clinical Presentation
Symptoms and Signs
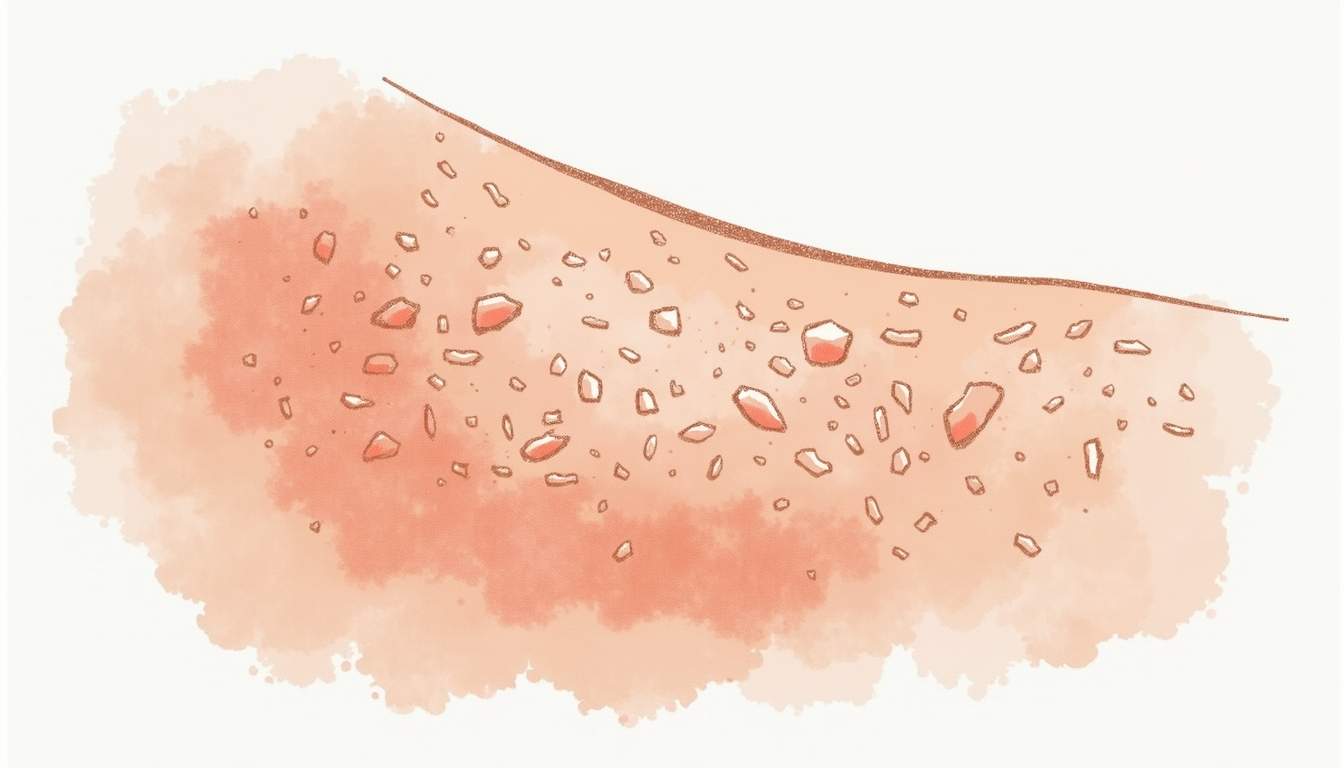
The hallmark of Pityriasis Versicolor is the appearance of discolored patches on the skin, which can range in color from light tan to dark brown or even pink. These patches are often more noticeable after sun exposure, as the surrounding skin may tan while the affected areas remain lighter. This can lead to a mottled appearance that some individuals find distressing.
In addition to discoloration, some individuals may experience mild itching or irritation, although many remain asymptomatic. The lesions typically occur on the trunk, shoulders, and upper arms, but they can also appear on the neck, face, and other areas of the body. The patches may be flat or slightly raised and can vary in size from small spots to larger areas of involvement.
Diagnosis
Diagnosing Pityriasis Versicolor typically involves a thorough clinical examination by a dermatologist. The physician will assess the appearance of the skin lesions and may inquire about the patient's medical history, including any previous episodes of similar skin changes. In some cases, a Wood's lamp examination may be performed, where the affected skin is illuminated with ultraviolet light, causing the lesions to fluoresce yellow-green.
Additionally, a skin scraping may be conducted to identify the presence of Malassezia yeast under a microscope. This diagnostic method helps confirm the diagnosis and rule out other skin conditions that may present similarly, such as vitiligo or seborrheic dermatitis.
Treatment Options
Topical Treatments
Topical antifungal agents are the first line of treatment for Pityriasis Versicolor. Commonly used medications include ketoconazole, clotrimazole, and selenium sulfide. These treatments work by reducing the yeast population on the skin and alleviating symptoms. Topical treatments are typically applied directly to the affected areas and may be used for several weeks to ensure complete resolution of the lesions.
In addition to antifungal creams and lotions, medicated shampoos containing selenium sulfide or zinc pyrithione can also be effective, particularly for lesions on the scalp or areas with hair. Patients are often advised to apply these shampoos to the affected areas and leave them on for a specified duration before rinsing.
Oral Medications
For more extensive or recurrent cases of Pityriasis Versicolor, oral antifungal medications may be prescribed. Commonly used oral agents include fluconazole and itraconazole. These medications are typically taken for a short duration, often a few days to a week, and are effective in clearing the yeast from the skin. Oral treatments may be necessary for individuals who do not respond to topical therapies or who experience frequent recurrences.
It is important for patients to follow their healthcare provider's instructions regarding dosage and duration of treatment, as improper use can lead to treatment failure or the development of drug resistance.
Prevention Strategies
Hygiene and Skin Care
Maintaining good hygiene and proper skin care is essential in preventing Pityriasis Versicolor. Individuals are encouraged to shower regularly, especially after sweating, to reduce the buildup of oils and yeast on the skin. Using non-comedogenic and oil-free skin care products can also help minimize the risk of yeast overgrowth.
Exfoliating the skin periodically may assist in removing dead skin cells and reducing the likelihood of yeast proliferation. However, individuals should avoid harsh scrubs that can irritate the skin, as this may exacerbate the condition.
Environmental Considerations
Since Pityriasis Versicolor is more common in warm and humid environments, individuals living in such climates should take additional precautions. Wearing loose-fitting, breathable clothing can help reduce sweating and moisture accumulation on the skin. Additionally, using air conditioning or fans to maintain a cooler environment can be beneficial.
During the warmer months, individuals may consider using antifungal body washes or shampoos as a preventive measure, especially if they have a history of recurrent Pityriasis Versicolor. Regular use of these products can help maintain a balanced skin flora and prevent the overgrowth of Malassezia yeast.
Conclusion
Pityriasis Versicolor is a common dermatological condition that can cause significant concern due to its impact on skin appearance. Understanding the etiology, clinical presentation, diagnosis, treatment options, and prevention strategies is crucial for effective management. While the condition is not harmful and is not contagious, its cosmetic implications can affect an individual's self-esteem and quality of life.
With appropriate treatment and preventive measures, individuals can effectively manage Pityriasis Versicolor and reduce the likelihood of recurrence. Consulting with a dermatologist for personalized advice and treatment options is recommended for anyone experiencing symptoms associated with this condition.
Visit Our Offices
Services:
- • Medical Dermatology
- • Surgical Dermatology
- • Laser Treatments
- • Cosmetic Dermatology
Services:
- • Medical Dermatology
- • Surgical Dermatology
- • Laser Treatments
- • Cosmetic Dermatology
Visit Our Offices
Services:
- • Medical Dermatology
- • Surgical Dermatology
- • Laser Treatments
- • Cosmetic Dermatology
Services:
- • Medical Dermatology
- • Surgical Dermatology
- • Laser Treatments
- • Cosmetic Dermatology