Introduction to Pilar Cysts
Pilar cysts, also known as trichilemmal cysts, are benign, fluid-filled sacs that typically develop on the scalp. They are often mistaken for other types of cysts or skin lesions, but their unique characteristics and origins set them apart. Pilar cysts are derived from hair follicles and are particularly common in individuals with a family history of such cysts. Understanding the formation, characteristics, and treatment options for pilar cysts is essential for both patients and healthcare providers.
These cysts are generally painless and slow-growing, making them a common occurrence in the population. While they can appear at any age, they are most frequently seen in adults, particularly women. Pilar cysts can vary in size, ranging from a few millimeters to several centimeters in diameter, and they may become inflamed or infected, leading to discomfort and the need for medical intervention.
In this glossary entry, we will explore the various aspects of pilar cysts, including their etiology, clinical presentation, diagnosis, treatment options, and potential complications. By gaining a comprehensive understanding of these cysts, individuals can better navigate their management and care.
Etiology of Pilar Cysts
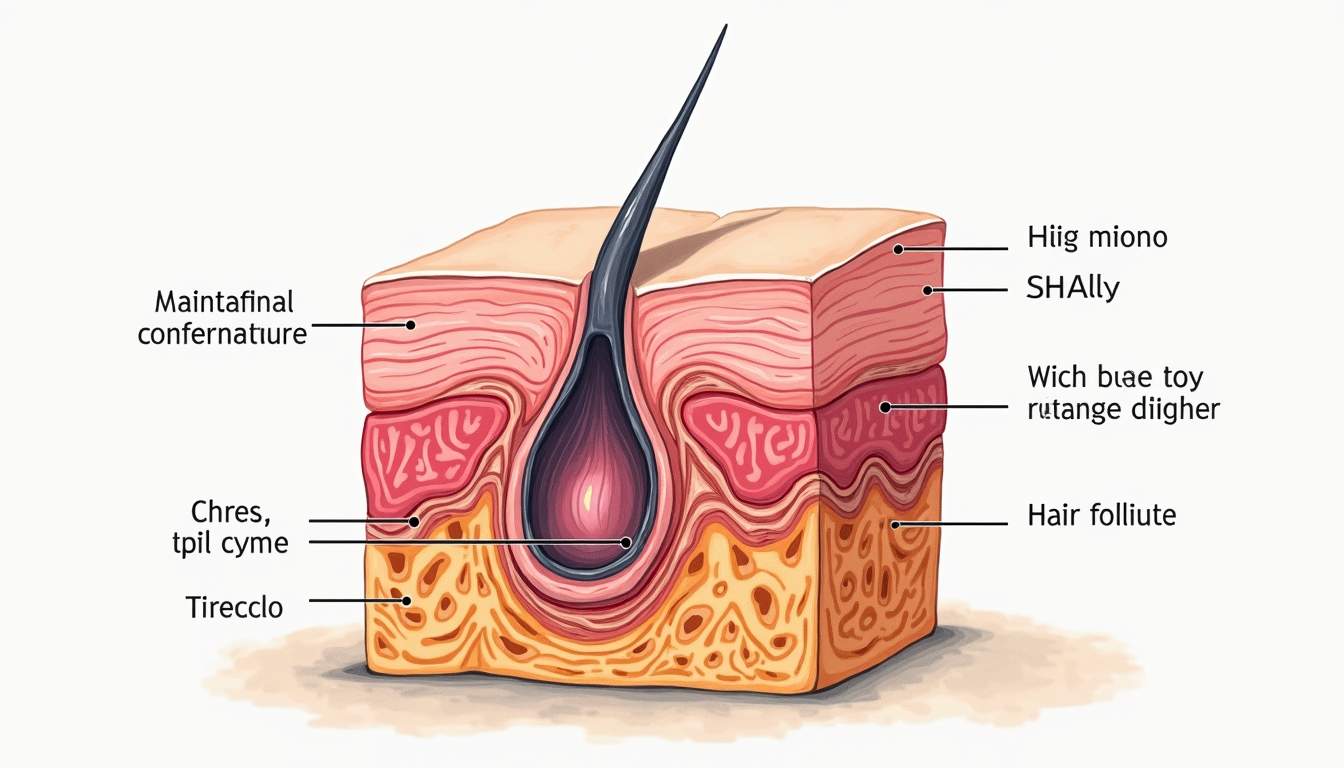
The etiology of pilar cysts is primarily linked to the abnormal proliferation of keratinocytes, the predominant cell type in the epidermis. These cysts arise from the outer root sheath of hair follicles, particularly those associated with terminal hair. The exact cause of this abnormal growth is not fully understood, but genetic predisposition plays a significant role. Studies have indicated that pilar cysts tend to run in families, suggesting a hereditary component.
Additionally, factors such as hormonal changes, particularly during puberty or pregnancy, may contribute to the development of pilar cysts. The presence of multiple cysts in an individual may indicate a condition known as steatocystoma multiplex, which is characterized by the formation of multiple sebaceous cysts, including pilar cysts. Environmental factors, such as trauma or irritation to the scalp, may also trigger the formation of these cysts in predisposed individuals.
Genetic Factors
Research has identified specific genetic mutations associated with the development of pilar cysts. The most notable is the mutation in the KRT17 gene, which encodes for keratin 17, a protein involved in the structural integrity of hair follicles. Individuals with a family history of pilar cysts may have an increased likelihood of developing these lesions due to inherited genetic factors.
Hormonal Influences
Hormonal influences, particularly androgens, may also play a role in the development of pilar cysts. These hormones can affect the growth and differentiation of keratinocytes, leading to the formation of cysts. This is particularly evident in women, as hormonal fluctuations during menstrual cycles, pregnancy, or menopause may contribute to the emergence of new cysts or the enlargement of existing ones.
Clinical Presentation
Pilar cysts typically present as smooth, firm, and round nodules that are often skin-colored or slightly yellowish. They are most commonly found on the scalp but can also occur on other areas of the body, such as the face, neck, and trunk. The cysts may vary in size, with some being small and barely noticeable, while others can grow to several centimeters in diameter.
While pilar cysts are usually asymptomatic, they can become inflamed or infected, leading to symptoms such as redness, tenderness, and drainage of pus or fluid. In some cases, the cysts may rupture, resulting in the release of keratin and other contents, which can cause localized inflammation and discomfort. It is essential for individuals to monitor their cysts for any changes in size, color, or symptoms, as these may indicate complications that require medical attention.
Common Symptoms
- Firm, round, movable nodules
- Skin-colored or yellowish appearance
- Asymptomatic in most cases
- Possible inflammation or infection
- Rupture leading to drainage of contents
Diagnosis of Pilar Cysts
The diagnosis of pilar cysts is primarily clinical, based on the characteristic appearance and location of the lesions. Dermatologists and healthcare providers typically perform a thorough physical examination, assessing the cysts for their size, shape, and consistency. In most cases, the diagnosis is straightforward, given the distinct features of pilar cysts.
In some instances, particularly when the cysts are atypical or when there is concern for malignancy, additional diagnostic measures may be warranted. These may include imaging studies, such as ultrasound or MRI, to evaluate the cyst's characteristics and surrounding structures. In rare cases, a biopsy may be performed to confirm the diagnosis and rule out other conditions, such as sebaceous adenomas or dermatofibromas.
Differential Diagnosis
When diagnosing pilar cysts, it is crucial to differentiate them from other skin lesions that may present similarly. Some common conditions that may be considered in the differential diagnosis include:
- Sebaceous cysts: These cysts arise from sebaceous glands and may contain sebum, while pilar cysts contain keratin.
- Dermatofibromas: These benign tumors are firm and may be mistaken for pilar cysts, but they typically have a different texture and may be associated with a dimple sign.
- Keratoacanthomas: These rapidly growing lesions can resemble pilar cysts but are typically more aggressive and require different management.
Treatment Options
The treatment of pilar cysts is often not necessary unless the cysts become symptomatic, infected, or cosmetically concerning to the individual. In such cases, several treatment options are available, ranging from conservative management to surgical intervention. The choice of treatment depends on the cyst's size, location, and symptoms, as well as the patient's preferences.
For asymptomatic cysts, observation may be the preferred approach. Regular monitoring can help ensure that any changes in the cyst's characteristics are promptly addressed. If the cyst becomes inflamed or infected, conservative measures such as warm compresses and antibiotics may be recommended to alleviate symptoms and prevent further complications.
Surgical Excision
Surgical excision is the definitive treatment for pilar cysts, particularly for those that are symptomatic or recurrent. The procedure involves removing the entire cyst along with its capsule to minimize the risk of recurrence. Surgical excision is typically performed under local anesthesia, and patients can expect a relatively quick recovery time. Post-operative care may include wound care instructions and follow-up appointments to monitor healing.
Other Treatment Modalities
In addition to surgical excision, other treatment modalities may be considered for pilar cysts. These may include:
- Drainage: In cases of infected cysts, drainage may be performed to relieve pressure and remove purulent material. However, this does not eliminate the cyst and may lead to recurrence.
- Intralesional corticosteroid injections: These injections may help reduce inflammation and promote healing in inflamed cysts, although they do not remove the cyst itself.
Potential Complications
While pilar cysts are generally benign and pose minimal risk to health, there are potential complications that individuals should be aware of. The most common complications include inflammation, infection, and recurrence after treatment. Infected cysts may require more aggressive management and can lead to scarring if not addressed promptly.
In rare cases, pilar cysts can become malignant, although this is extremely uncommon. The risk of malignancy is higher in individuals with a history of skin cancer or other risk factors. Therefore, it is essential for individuals with pilar cysts to monitor their lesions for any changes and seek medical advice if they notice any concerning symptoms.
Monitoring and Follow-Up
Regular monitoring of pilar cysts is crucial for individuals with a history of these lesions. Follow-up appointments with a dermatologist can help ensure that any changes in the cyst's characteristics are promptly addressed. Patients should be educated on the signs and symptoms of complications, such as increased redness, swelling, or drainage, and encouraged to seek medical attention if these occur.
Conclusion
Pilar cysts are common dermatological lesions that are generally benign and asymptomatic. Understanding their etiology, clinical presentation, diagnosis, treatment options, and potential complications is essential for effective management. While most individuals with pilar cysts do not require treatment, those with symptomatic or recurrent cysts can benefit from surgical excision or other therapeutic interventions.
By fostering awareness and knowledge about pilar cysts, individuals can take proactive steps in monitoring their skin health and seeking appropriate care when necessary. As research continues to evolve in the field of dermatology, further insights into the genetic and environmental factors contributing to pilar cysts may enhance our understanding and management of these common skin lesions.
Visit Our Offices
Services:
- • Medical Dermatology
- • Surgical Dermatology
- • Laser Treatments
- • Cosmetic Dermatology
Services:
- • Medical Dermatology
- • Surgical Dermatology
- • Laser Treatments
- • Cosmetic Dermatology
Visit Our Offices
Services:
- • Medical Dermatology
- • Surgical Dermatology
- • Laser Treatments
- • Cosmetic Dermatology
Services:
- • Medical Dermatology
- • Surgical Dermatology
- • Laser Treatments
- • Cosmetic Dermatology