Melanocyte-stimulating Hormone: Dermatology Explained
Melanocyte-stimulating hormone (MSH) is a peptide hormone produced by the pituitary that stimulates melanin production in melanocytes to regulate pigmentation and also influences appetite and energy balance.
Introduction to Melanocyte-stimulating Hormone (MSH)
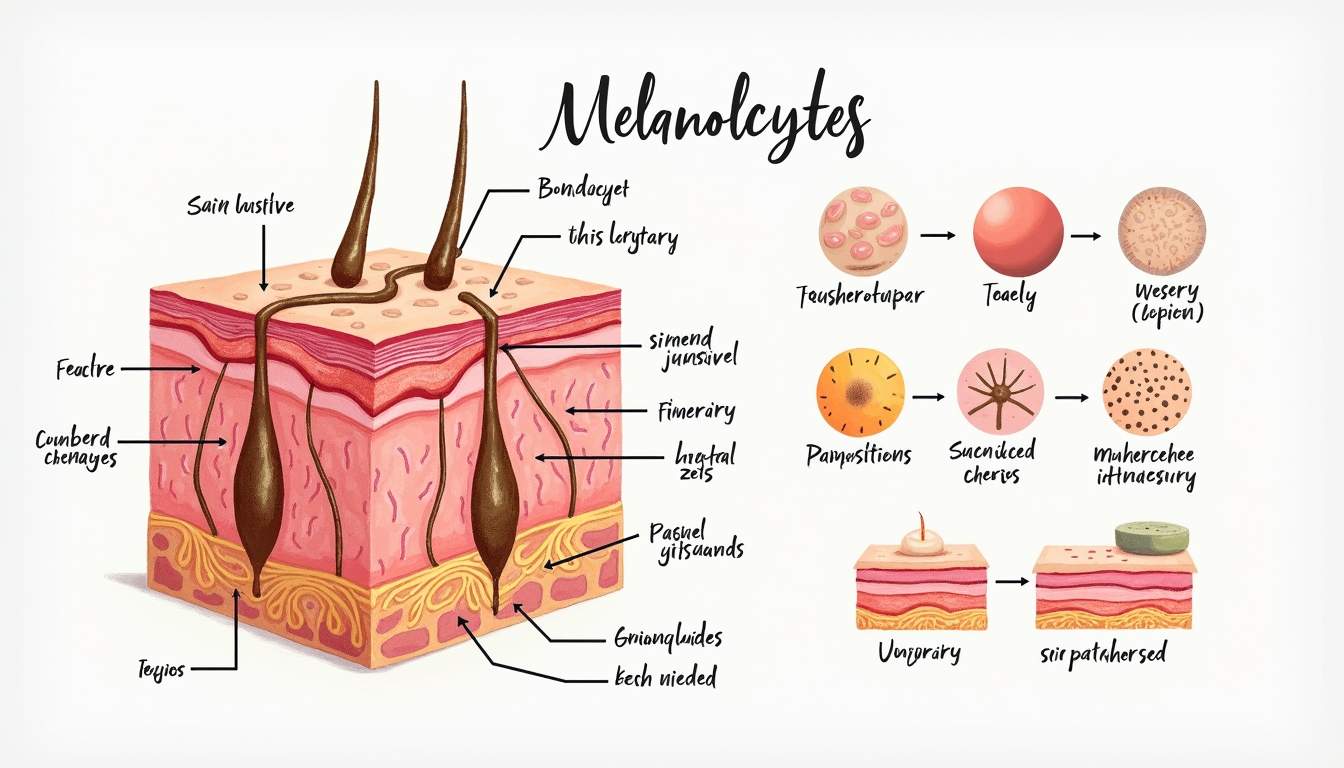
Melanocyte-stimulating hormone (MSH) is a peptide hormone produced by the anterior pituitary gland, which plays a crucial role in the regulation of skin pigmentation. MSH is part of the pro-opiomelanocortin (POMC) family of hormones, which also includes adrenocorticotropic hormone (ACTH) and beta-endorphins. The primary function of MSH is to stimulate the production and release of melanin from melanocytes, the specialized cells responsible for skin, hair, and eye pigmentation.
In dermatology, understanding the role of MSH is vital for comprehending various skin conditions, pigmentation disorders, and the overall physiology of the skin. MSH influences not only pigmentation but also has effects on appetite regulation, energy homeostasis, and immune response. The intricate relationship between MSH and skin health underscores the importance of this hormone in dermatological research and clinical practice.
This glossary entry aims to provide a comprehensive overview of MSH, its biological functions, its role in dermatology, and its implications in various skin conditions. By exploring the multifaceted aspects of MSH, we can better appreciate its significance in both health and disease.
Biological Functions of Melanocyte-stimulating Hormone
Production and Secretion
MSH is synthesized and secreted by the melanotropic cells of the anterior pituitary gland. The production of MSH is regulated by various factors, including environmental stimuli such as ultraviolet (UV) radiation exposure. When the skin is exposed to UV light, it triggers the release of MSH, which in turn stimulates melanocytes to produce more melanin, leading to tanning of the skin as a protective response against UV damage.
In addition to UV exposure, other factors such as hormonal changes, stress, and certain medications can influence MSH levels. For instance, during pregnancy, increased levels of estrogen can lead to elevated MSH levels, contributing to the development of melasma, a common skin condition characterized by dark patches on the face.
MSH exists in several forms, including alpha-MSH, beta-MSH, and gamma-MSH, each with distinct biological activities. Alpha-MSH is the most studied form and is primarily responsible for stimulating melanin production. Beta-MSH and gamma-MSH have additional roles in appetite regulation and inflammation, showcasing the diverse functions of this hormone.
Mechanism of Action
The action of MSH is mediated through its interaction with specific receptors known as melanocortin receptors (MCRs), which are G-protein coupled receptors located on the surface of melanocytes. There are five known subtypes of melanocortin receptors: MC1R, MC2R, MC3R, MC4R, and MC5R, each playing different roles in the body. MC1R is particularly significant in the context of skin pigmentation, as its activation leads to increased melanin synthesis.
When MSH binds to MC1R on melanocytes, it activates a signaling cascade that results in the upregulation of enzymes involved in melanin production, such as tyrosinase. This process not only enhances melanin synthesis but also promotes the transfer of melanin granules to surrounding keratinocytes, contributing to the overall pigmentation of the skin.
Furthermore, MSH has been shown to possess anti-inflammatory properties, which may play a role in skin health by modulating immune responses and reducing inflammation in various dermatological conditions. This dual role of MSH as both a pigment regulator and an anti-inflammatory agent highlights its importance in maintaining skin homeostasis.
Role of MSH in Dermatological Conditions
Hyperpigmentation Disorders
Hyperpigmentation disorders are characterized by an excess production of melanin, leading to darker patches on the skin. Conditions such as melasma, post-inflammatory hyperpigmentation, and lentigines are influenced by MSH levels. In melasma, for instance, increased MSH production can result from hormonal changes, particularly during pregnancy or with the use of oral contraceptives, leading to the characteristic brown patches on the face.
Post-inflammatory hyperpigmentation occurs following skin injuries, such as acne or eczema, where MSH is released in response to inflammation, stimulating melanocytes to produce excess melanin. Understanding the role of MSH in these conditions is crucial for developing effective treatment strategies, which may include topical agents that inhibit melanin production or procedures like chemical peels and laser therapy.
Additionally, certain genetic factors, such as variations in the MC1R gene, can predispose individuals to hyperpigmentation disorders. These genetic predispositions can influence how the skin responds to MSH and other pigmentation stimuli, further complicating the management of these conditions.
Hypopigmentation Disorders
Conversely, hypopigmentation disorders, such as vitiligo and albinism, are characterized by a deficiency in melanin production. In vitiligo, the loss of melanocytes leads to white patches on the skin, and while MSH is typically elevated in response to skin damage, its effectiveness is diminished due to the absence of functional melanocytes. This presents a challenge in treating vitiligo, as stimulating melanin production through MSH may not yield the desired results.
Albinism is a genetic condition resulting from mutations that affect melanin production, leading to a lack of pigmentation in the skin, hair, and eyes. Individuals with albinism often have reduced levels of MSH due to the underlying genetic defects affecting melanocyte function. Understanding the role of MSH in these conditions can aid in developing targeted therapies that address the underlying mechanisms of hypopigmentation.
Research into the potential therapeutic applications of MSH analogs or agonists is ongoing, with the hope of finding effective treatments for individuals suffering from hypopigmentation disorders. By harnessing the knowledge of MSH's role in pigmentation, dermatologists can explore innovative approaches to restore skin color and improve the quality of life for affected individuals.
MSH and Skin Aging
Impact of Aging on MSH Levels
As individuals age, various physiological changes occur, including alterations in hormone levels. MSH is no exception, as studies have shown that MSH levels may decline with age, potentially contributing to changes in skin pigmentation and overall skin health. This decline in MSH may lead to reduced melanin production, resulting in a more uneven skin tone and increased susceptibility to UV damage.
Additionally, the aging process is associated with a decrease in the number and function of melanocytes, further exacerbating the effects of reduced MSH levels. The combination of these factors can lead to the development of age-related pigmentation changes, such as solar lentigines, commonly known as age spots.
Understanding the relationship between MSH and skin aging is essential for developing anti-aging strategies that focus on maintaining healthy pigmentation and protecting the skin from environmental damage. This may involve lifestyle modifications, such as sun protection and a balanced diet, as well as potential therapeutic interventions targeting MSH signaling pathways.
Potential Therapeutic Approaches
Given the multifaceted roles of MSH in skin health, researchers are exploring various therapeutic approaches to harness its potential benefits. One area of interest is the development of MSH analogs that can mimic the hormone's effects on melanocytes, potentially providing a means to treat both hyperpigmentation and hypopigmentation disorders.
Topical formulations containing MSH or its analogs may offer a novel approach to stimulate melanin production in individuals with hypopigmentation disorders, while also providing protective effects against UV damage. Additionally, understanding the anti-inflammatory properties of MSH may lead to the development of new treatments for inflammatory skin conditions, such as psoriasis and eczema.
Furthermore, lifestyle interventions that promote healthy skin aging, such as regular sun protection, a balanced diet rich in antioxidants, and adequate hydration, can complement any pharmacological treatments aimed at modulating MSH levels. By adopting a holistic approach to skin health, individuals can optimize their skin's appearance and function as they age.
Conclusion
Melanocyte-stimulating hormone (MSH) is a critical player in the regulation of skin pigmentation and overall skin health. Its complex interactions with melanocytes and various signaling pathways highlight its importance in dermatology. Understanding the biological functions of MSH, its role in dermatological conditions, and the implications of aging on its levels can provide valuable insights for both clinicians and patients.
As research continues to uncover the intricacies of MSH and its potential therapeutic applications, dermatologists can look forward to innovative strategies for managing pigmentation disorders and promoting healthy skin aging. By recognizing the significance of MSH in skin physiology, we can enhance our understanding of dermatological conditions and improve patient care.
In summary, MSH is not merely a pigment regulator; it is a multifaceted hormone with implications that extend beyond pigmentation, influencing various aspects of skin health and disease. The ongoing exploration of MSH's functions and therapeutic potential will undoubtedly shape the future of dermatology, paving the way for more effective treatments and improved outcomes for patients.
Visit Our Offices
Services:
- • Medical Dermatology
- • Surgical Dermatology
- • Laser Treatments
- • Cosmetic Dermatology
Services:
- • Medical Dermatology
- • Surgical Dermatology
- • Laser Treatments
- • Cosmetic Dermatology
Visit Our Offices
Services:
- • Medical Dermatology
- • Surgical Dermatology
- • Laser Treatments
- • Cosmetic Dermatology
Services:
- • Medical Dermatology
- • Surgical Dermatology
- • Laser Treatments
- • Cosmetic Dermatology