Introduction to Lichen Simplex Chronicus
Lichen Simplex Chronicus (LSC) is a dermatological condition characterized by the chronic itching and scratching of the skin, leading to thickened, leathery patches. This condition often arises as a response to chronic irritation or trauma to the skin, which may be due to various factors such as stress, allergies, or underlying skin disorders. Understanding LSC is crucial for both patients and healthcare providers, as it can significantly impact the quality of life and may be indicative of other underlying issues.
The term "lichen" refers to a type of skin lesion that resembles a lichen, a symbiotic organism composed of fungi and algae, while "simplex" indicates its uncomplicated nature. "Chronicus" signifies the long-lasting nature of the condition. LSC is not a standalone diagnosis but rather a manifestation of an underlying issue, often requiring a comprehensive approach to management and treatment.
In this glossary entry, we will explore the etiology, clinical features, diagnosis, treatment options, and potential complications associated with Lichen Simplex Chronicus, providing a thorough understanding of this dermatological condition.
Etiology of Lichen Simplex Chronicus
Causes and Risk Factors
The etiology of Lichen Simplex Chronicus is multifactorial, involving both intrinsic and extrinsic factors that contribute to the development of the condition. Chronic itching is often the primary trigger, which may stem from various sources such as eczema, psoriasis, or contact dermatitis. The cycle of itching and scratching leads to further skin damage, creating a vicious cycle that perpetuates the condition.
Several risk factors have been identified that may predispose individuals to LSC, including:
- Atopic Dermatitis: Individuals with a history of atopic dermatitis are more likely to develop LSC due to the chronic nature of their skin condition.
- Psychological Stress: Emotional stress can exacerbate itching and scratching behaviors, leading to the development of LSC.
- Skin Irritation: Frequent exposure to irritants, such as soaps, detergents, or certain fabrics, can trigger the onset of LSC.
- Genetic Predisposition: A family history of skin conditions may increase the likelihood of developing LSC.
Pathophysiology
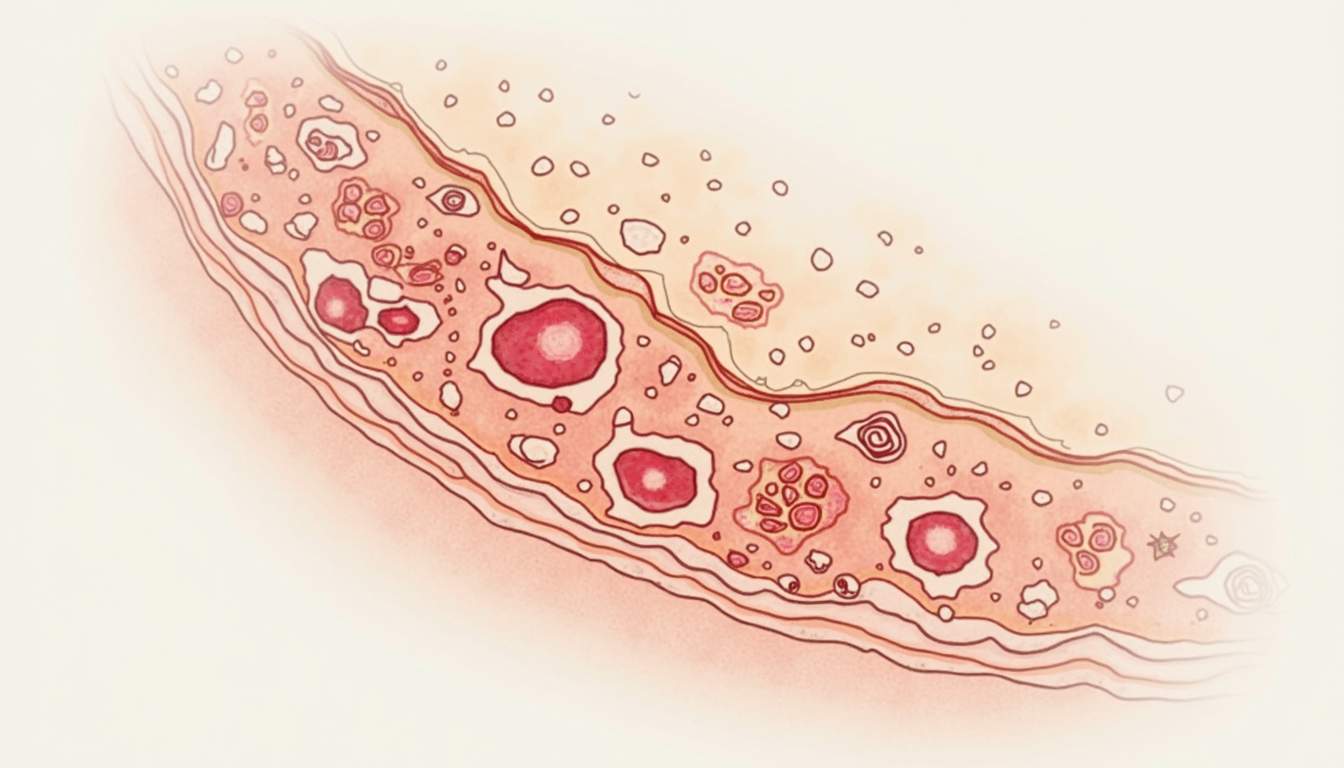
The pathophysiology of Lichen Simplex Chronicus involves a complex interplay between the nervous system and the skin. Chronic scratching leads to a phenomenon known as "lichenification," where the skin becomes thickened and leathery due to repeated trauma. This thickening is a result of hyperplasia of the epidermis and dermis, which alters the skin's barrier function and contributes to further irritation.
Additionally, neurogenic inflammation plays a significant role in LSC. The release of neuropeptides and pro-inflammatory cytokines in response to chronic itching can lead to increased sensitivity and further exacerbate the itching-scratching cycle. This neurogenic component highlights the importance of addressing both the physical and psychological aspects of the condition in treatment.
Clinical Features of Lichen Simplex Chronicus
Symptoms
The hallmark symptom of Lichen Simplex Chronicus is intense itching, which can be persistent and debilitating. Patients often report that the itching worsens at night or during periods of stress, leading to sleep disturbances and decreased quality of life. The urge to scratch can become overwhelming, and individuals may find themselves engaging in compulsive scratching behaviors.
In terms of physical examination, LSC typically presents as well-defined, thickened plaques of skin that may vary in color from red to brown. These plaques often have a shiny appearance and may be covered with scales or crusts due to secondary infections or excoriations. Common sites for LSC include the neck, scalp, wrists, ankles, and the inner thighs, although it can occur anywhere on the body.
Associated Conditions
Lichen Simplex Chronicus is often associated with other dermatological conditions, particularly those that involve chronic itching. Conditions such as eczema, psoriasis, and scabies can lead to the development of LSC as patients scratch to relieve their discomfort. Additionally, psychological conditions such as anxiety and depression may coexist with LSC, further complicating the management of the condition.
It is also important to note that LSC can sometimes be mistaken for other skin disorders, such as lichen planus or psoriasis, due to similar clinical presentations. Therefore, a thorough clinical evaluation is essential to differentiate LSC from these conditions and to ensure appropriate management.
Diagnosis of Lichen Simplex Chronicus
Clinical Evaluation
The diagnosis of Lichen Simplex Chronicus is primarily clinical, based on the characteristic history and physical examination findings. Dermatologists will typically assess the patient's history of itching, scratching behaviors, and any associated skin conditions. A detailed history can provide insights into potential triggers, including stressors, irritants, or underlying skin diseases.
During the physical examination, dermatologists will look for the characteristic thickened plaques and assess their distribution on the body. The appearance of the skin, along with the patient's reported symptoms, usually allows for a confident diagnosis of LSC. In some cases, a skin biopsy may be performed to rule out other conditions, particularly if the diagnosis is uncertain.
Diagnostic Tests
While the diagnosis of Lichen Simplex Chronicus is primarily clinical, certain diagnostic tests may be utilized to exclude other dermatological conditions. These tests may include:
- Skin Biopsy: A small sample of skin may be taken to examine under a microscope, helping to differentiate LSC from conditions like lichen planus or psoriasis.
- Patch Testing: If contact dermatitis is suspected as a contributing factor, patch testing may be performed to identify specific allergens or irritants.
- Laboratory Tests: In cases where systemic conditions are suspected, blood tests may be conducted to evaluate for underlying issues such as thyroid dysfunction or autoimmune diseases.
Treatment Options for Lichen Simplex Chronicus
Topical Therapies
The primary goal of treatment for Lichen Simplex Chronicus is to break the cycle of itching and scratching. Topical therapies are often the first line of treatment and may include:
- Topical Corticosteroids: These anti-inflammatory medications can help reduce itching and inflammation. High-potency corticosteroids may be prescribed for thickened plaques, while lower-potency options may be used for sensitive areas.
- Calcineurin Inhibitors: Medications such as tacrolimus or pimecrolimus can be effective in reducing inflammation and itching, particularly in sensitive areas where corticosteroids may not be suitable.
- Moisturizers: Regular use of emollients can help restore the skin barrier and reduce dryness, which may contribute to itching.
Systemic Therapies
In cases where topical treatments are insufficient, systemic therapies may be considered. These may include:
- Oral Corticosteroids: Short courses of oral corticosteroids may be prescribed for severe cases to quickly reduce inflammation and itching.
- Antihistamines: Oral antihistamines can help alleviate itching, particularly if there is an allergic component to the condition.
- Psychotropic Medications: In cases where psychological factors play a significant role, medications such as selective serotonin reuptake inhibitors (SSRIs) may be beneficial in managing anxiety or depression.
Behavioral Interventions
Behavioral interventions are crucial in the management of Lichen Simplex Chronicus. Patients are often encouraged to engage in strategies to reduce scratching behaviors, which may include:
- Behavioral Therapy: Cognitive-behavioral therapy (CBT) can help patients develop coping strategies to manage stress and reduce the urge to scratch.
- Habit Reversal Training: This technique involves identifying triggers for scratching and replacing the behavior with a competing response.
- Relaxation Techniques: Mindfulness, meditation, and other relaxation techniques can help reduce stress and anxiety, which may contribute to itching.
Potential Complications of Lichen Simplex Chronicus
Secondary Infections
One of the most common complications associated with Lichen Simplex Chronicus is the development of secondary infections. Chronic scratching can break the skin barrier, making it susceptible to bacterial, viral, or fungal infections. Conditions such as impetigo, folliculitis, or tinea can arise as a result of skin trauma, necessitating prompt treatment to prevent further complications.
Patients with LSC should be educated on the signs of infection, which may include increased redness, swelling, warmth, and the presence of pus or crusting. Early recognition and treatment of infections are essential to prevent complications and promote healing.
Psychosocial Impact
The psychosocial impact of Lichen Simplex Chronicus can be significant. The chronic nature of the condition, coupled with the distressing symptoms of itching and discomfort, can lead to feelings of frustration, anxiety, and depression. Patients may experience social withdrawal, decreased self-esteem, and impaired quality of life due to the visible nature of the skin lesions and the associated itching.
Addressing the psychological aspects of LSC is vital in the overall management of the condition. Support groups, counseling, and therapy can provide patients with coping strategies and emotional support, helping them to navigate the challenges associated with living with a chronic skin condition.
Conclusion
Lichen Simplex Chronicus is a complex dermatological condition that requires a multifaceted approach to diagnosis and management. Understanding the etiology, clinical features, and treatment options is crucial for both patients and healthcare providers. By addressing the underlying causes of itching and implementing effective treatment strategies, individuals with LSC can achieve significant improvement in their symptoms and overall quality of life.
As research continues to evolve in the field of dermatology, ongoing education and awareness about conditions like Lichen Simplex Chronicus will be essential in providing optimal care for patients. Collaborative efforts between dermatologists, mental health professionals, and patients themselves can lead to more effective management strategies and improved outcomes.
Visit Our Offices
Services:
- • Medical Dermatology
- • Surgical Dermatology
- • Laser Treatments
- • Cosmetic Dermatology
Services:
- • Medical Dermatology
- • Surgical Dermatology
- • Laser Treatments
- • Cosmetic Dermatology
Visit Our Offices
Services:
- • Medical Dermatology
- • Surgical Dermatology
- • Laser Treatments
- • Cosmetic Dermatology
Services:
- • Medical Dermatology
- • Surgical Dermatology
- • Laser Treatments
- • Cosmetic Dermatology