Introduction to Keratosis Pilaris
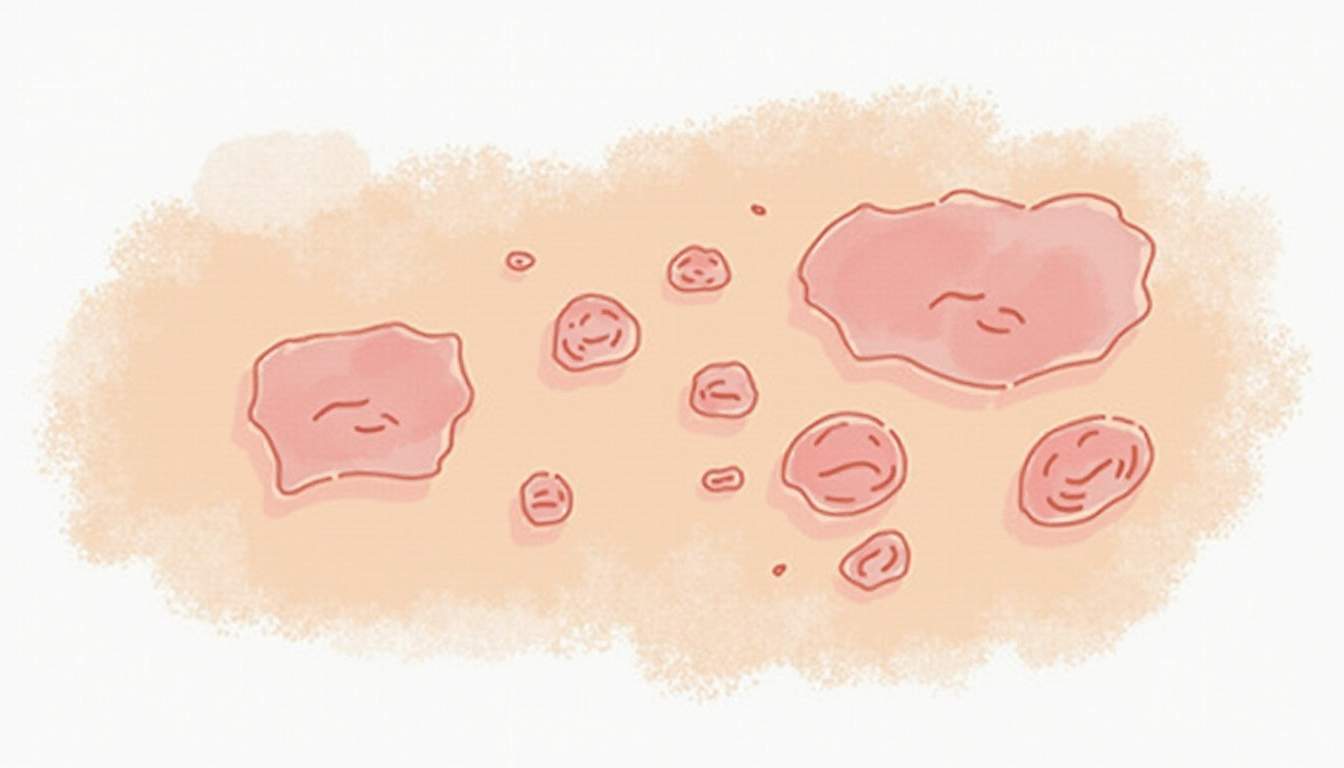
Keratosis pilaris (KP) is a common skin condition characterized by the appearance of small, rough, and often red or white bumps on the skin. These bumps are typically found on the upper arms, thighs, cheeks, and buttocks, although they can occur anywhere on the body except for the palms and soles. The condition is caused by the buildup of keratin, a protein that protects the skin from infections and other harmful substances. In keratosis pilaris, the keratin forms hard plugs within the hair follicles, leading to the characteristic bumps.
While keratosis pilaris is not harmful and does not pose any health risks, it can be a source of cosmetic concern for many individuals. Understanding the underlying mechanisms, causes, and treatment options for keratosis pilaris can help those affected manage the condition more effectively and improve their skin's appearance.
This glossary entry aims to provide a comprehensive overview of keratosis pilaris, including its symptoms, causes, risk factors, diagnosis, treatment options, and prevention strategies. By delving into these aspects, we hope to equip readers with the knowledge necessary to understand and address this common dermatological condition.
Symptoms of Keratosis Pilaris
The primary symptom of keratosis pilaris is the presence of small, raised bumps on the skin. These bumps may vary in color from skin-toned to red or white and are often most noticeable on the upper arms, thighs, and cheeks. In some cases, the bumps may be accompanied by mild itching or irritation, although this is not always the case. The texture of the skin in affected areas can feel rough or sandpaper-like due to the accumulation of keratin.
In addition to the physical appearance of the bumps, individuals with keratosis pilaris may experience emotional or psychological effects. The visibility of the condition can lead to self-consciousness, embarrassment, or frustration, particularly in social situations or during warmer months when skin is more exposed. It is important to note that keratosis pilaris is a benign condition and does not cause pain or other serious health issues.
In some instances, keratosis pilaris may improve with age, as the skin undergoes natural changes. However, for many individuals, the condition persists throughout life, necessitating ongoing management and care.
Causes of Keratosis Pilaris
Keratin Buildup
The primary cause of keratosis pilaris is the overproduction of keratin, a fibrous protein that is a key component of the skin, hair, and nails. In individuals with KP, keratin accumulates in the hair follicles, leading to the formation of small, hard plugs. This buildup can occur for various reasons, including genetic predisposition, skin type, and environmental factors.
Keratin is essential for protecting the skin from external elements, but when produced in excess, it can lead to blockages in the hair follicles. This blockage prevents hair from emerging properly, resulting in the characteristic bumps associated with keratosis pilaris. The exact mechanism behind this overproduction is not fully understood, but it is believed to involve a combination of genetic and environmental influences.
Genetic Factors
Research indicates that keratosis pilaris has a hereditary component, meaning it can run in families. If one or both parents have experienced KP, their children are more likely to develop the condition as well. Genetic factors may influence the skin's ability to shed dead skin cells and regulate keratin production, leading to the characteristic symptoms of keratosis pilaris.
While genetics play a significant role, it is important to note that not everyone with a family history of keratosis pilaris will develop the condition. Environmental factors, skin type, and individual differences in skin physiology also contribute to the likelihood of developing KP.
Risk Factors for Keratosis Pilaris
Several risk factors can increase an individual's likelihood of developing keratosis pilaris. Understanding these factors can help individuals identify their risk and take proactive measures to manage the condition. The following are some common risk factors associated with keratosis pilaris:
- Family History: As mentioned earlier, a family history of keratosis pilaris increases the likelihood of developing the condition.
- Age: Keratosis pilaris is more commonly observed in children and adolescents, although it can persist into adulthood.
- Skin Type: Individuals with dry or sensitive skin are more prone to keratosis pilaris, as their skin may have difficulty shedding dead skin cells effectively.
- Seasonal Changes: KP symptoms may worsen during the winter months when the air is dry, leading to increased skin dryness and irritation.
Diagnosis of Keratosis Pilaris
Diagnosing keratosis pilaris typically involves a thorough examination of the skin by a qualified dermatologist. The doctor will assess the appearance of the bumps, their location, and any associated symptoms. In most cases, a visual inspection is sufficient for diagnosis, as keratosis pilaris has distinct characteristics that differentiate it from other skin conditions.
In rare instances, a dermatologist may perform a skin biopsy to rule out other conditions that may present similarly, such as folliculitis or acne. However, this is generally unnecessary for typical cases of keratosis pilaris. If the diagnosis is confirmed, the dermatologist will discuss potential treatment options and management strategies tailored to the individual's needs.
Treatment Options for Keratosis Pilaris
Topical Treatments
While there is no cure for keratosis pilaris, several topical treatments can help manage the condition and improve the skin's appearance. These treatments often focus on exfoliating the skin, reducing keratin buildup, and moisturizing the affected areas. Common topical treatments include:
- Exfoliating Creams: Creams containing alpha hydroxy acids (AHAs) or beta hydroxy acids (BHAs) can help exfoliate the skin and promote the shedding of dead skin cells. Ingredients such as glycolic acid and salicylic acid are commonly used in these formulations.
- Urea Creams: Urea is a powerful humectant that helps to soften and hydrate the skin. Urea creams can also aid in breaking down keratin plugs, making them effective for treating keratosis pilaris.
- Retinoids: Topical retinoids, such as tretinoin, can help improve skin cell turnover and reduce keratin buildup. However, these treatments may cause irritation, so they should be used under the guidance of a dermatologist.
Moisturizers
In addition to exfoliating treatments, regular use of moisturizers is essential for managing keratosis pilaris. Keeping the skin hydrated can help reduce dryness and irritation, which may exacerbate the condition. Look for moisturizers that contain ingredients such as ceramides, glycerin, or hyaluronic acid, as these can provide effective hydration and support the skin's barrier function.
Applying moisturizer immediately after bathing or showering can help lock in moisture and prevent the skin from becoming overly dry. Consistency is key, as regular use of moisturizers can lead to noticeable improvements in the skin's texture and appearance over time.
Prevention Strategies for Keratosis Pilaris
While keratosis pilaris cannot be entirely prevented, certain strategies can help minimize the severity of the condition and reduce flare-ups. Implementing these preventive measures can lead to healthier skin and improved overall appearance:
- Gentle Exfoliation: Regularly exfoliating the skin using gentle scrubs or exfoliating gloves can help remove dead skin cells and prevent keratin buildup. However, avoid harsh scrubs that can irritate the skin.
- Moisturize Regularly: Consistent use of moisturizers can help maintain skin hydration and prevent dryness, which can worsen keratosis pilaris.
- Avoid Hot Showers: Hot water can strip the skin of its natural oils, leading to dryness. Opt for lukewarm showers and limit bath time to help preserve skin moisture.
- Wear Breathable Fabrics: Choose loose-fitting, breathable clothing made from natural fibers to reduce friction and irritation on the skin.
Conclusion
Keratosis pilaris is a common and benign skin condition that affects many individuals. While it can be a source of cosmetic concern, understanding the causes, symptoms, and treatment options can empower those affected to manage the condition effectively. By implementing appropriate skincare routines and preventive measures, individuals can improve their skin's appearance and reduce the impact of keratosis pilaris on their lives.
For those struggling with keratosis pilaris, consulting a dermatologist can provide personalized guidance and treatment recommendations tailored to individual needs. With the right approach, it is possible to achieve smoother, healthier skin and enhance overall confidence.
Visit Our Offices
Services:
- • Medical Dermatology
- • Surgical Dermatology
- • Laser Treatments
- • Cosmetic Dermatology
Services:
- • Medical Dermatology
- • Surgical Dermatology
- • Laser Treatments
- • Cosmetic Dermatology
Visit Our Offices
Services:
- • Medical Dermatology
- • Surgical Dermatology
- • Laser Treatments
- • Cosmetic Dermatology
Services:
- • Medical Dermatology
- • Surgical Dermatology
- • Laser Treatments
- • Cosmetic Dermatology