Introduction to Keratinocytes
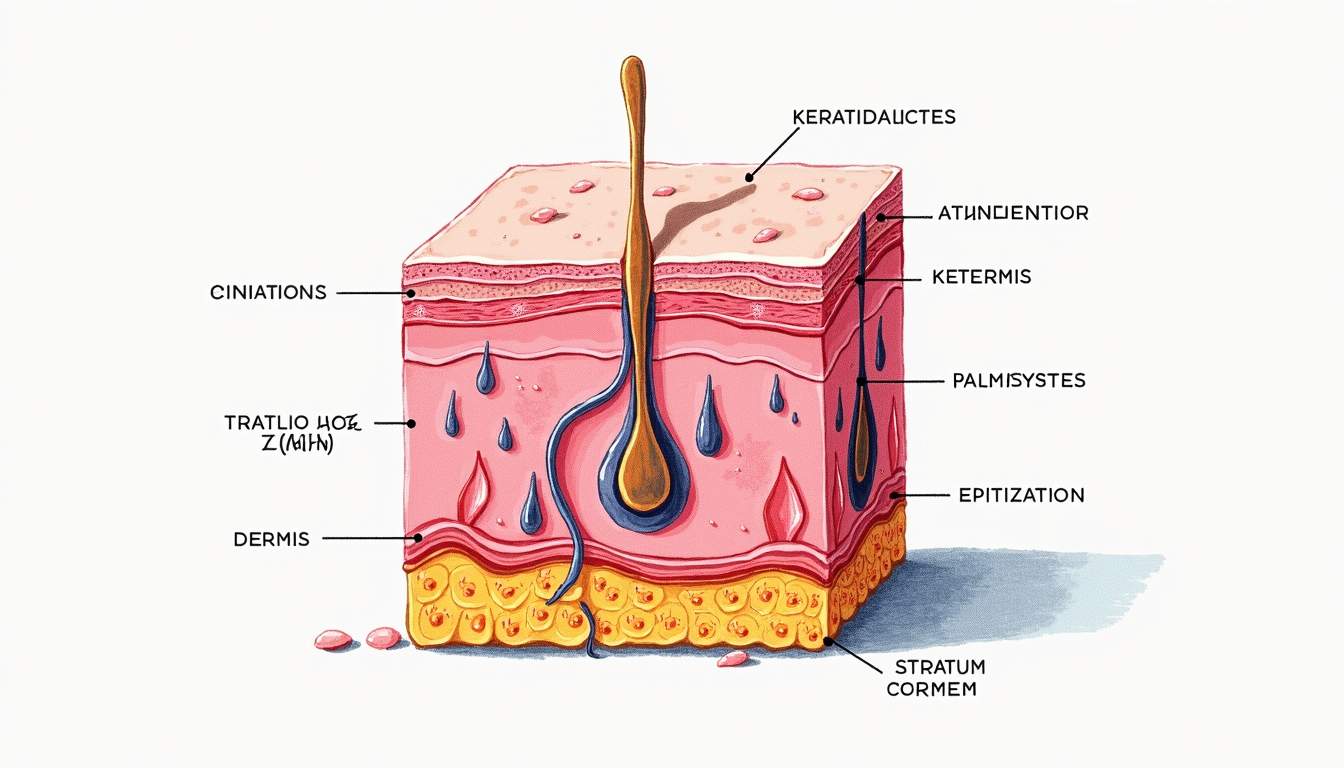
Keratinocytes are the primary cell type found in the epidermis, the outermost layer of the skin. They play a crucial role in the skin's barrier function, protecting the body from environmental hazards such as pathogens, chemicals, and physical injuries. These cells are responsible for the production of keratin, a fibrous protein that provides strength and resilience to the skin. Understanding keratinocytes is essential for comprehending various dermatological conditions and the overall health of the skin.
Keratinocytes originate from stem cells located in the basal layer of the epidermis. As they mature, they undergo a process known as keratinization, where they gradually move upward through the layers of the epidermis, becoming more flattened and filled with keratin. This process is vital for maintaining the integrity of the skin and ensuring its protective functions. The lifecycle of keratinocytes is typically around 28 days, although this can vary based on several factors, including age, skin type, and environmental influences.
In addition to their structural role, keratinocytes are also involved in various biological processes, including immune response, wound healing, and the regulation of skin hydration. They communicate with other skin cells, such as melanocytes and Langerhans cells, to maintain skin homeostasis and respond to injury or infection. The study of keratinocytes is a significant area of research in dermatology, as abnormalities in their function can lead to various skin disorders.
The Structure of Keratinocytes
Cellular Composition
Keratinocytes are characterized by their unique structure, which is adapted to their function in the epidermis. They are polygonal in shape and contain a nucleus, cytoplasm, and various organelles, including mitochondria, endoplasmic reticulum, and Golgi apparatus. The most notable feature of keratinocytes is their ability to produce keratin, which is synthesized in the cytoplasm and eventually accumulates in the cell's outer layers.
Keratinocytes can be classified into several types based on their location within the epidermis. The basal keratinocytes, found in the deepest layer, are cuboidal and actively divide to replenish the skin's surface. As they move upward, they transition into spinous keratinocytes, which are larger and more flattened. Finally, they become granular keratinocytes, which contain keratohyalin granules that contribute to the keratinization process.
The outermost layer of keratinocytes, known as the stratum corneum, consists of dead, flattened cells that are rich in keratin. This layer acts as a barrier to prevent water loss and protect against external aggressors. The continuous turnover of keratinocytes ensures that the skin remains healthy and functional, highlighting the importance of these cells in maintaining skin integrity.
Keratinization Process
The keratinization process is a complex series of events that keratinocytes undergo as they migrate from the basal layer to the skin's surface. This process begins with the proliferation of basal keratinocytes, which divide and produce new cells. As these cells move upward, they begin to differentiate and undergo several morphological changes.
During keratinization, keratinocytes produce various proteins, including keratins and filaggrin, which play essential roles in forming the skin barrier. The cells also lose their nuclei and organelles, becoming more flattened and filled with keratin. This transformation is crucial for the formation of the stratum corneum, which provides the skin with its protective properties.
The regulation of keratinization is influenced by several factors, including hormonal changes, environmental conditions, and skin disorders. Abnormalities in this process can lead to various skin conditions, such as psoriasis, eczema, and ichthyosis, highlighting the importance of understanding keratinocyte biology in dermatology.
Functions of Keratinocytes
Barrier Function
One of the primary functions of keratinocytes is to form a barrier that protects the underlying tissues from external insults. The stratum corneum, composed of dead keratinocytes, acts as a physical barrier that prevents the entry of pathogens, allergens, and harmful substances. Additionally, it helps to retain moisture within the skin, preventing dehydration and maintaining hydration levels.
The barrier function of keratinocytes is further enhanced by the production of lipids, such as ceramides, cholesterol, and fatty acids, which are secreted into the extracellular space. These lipids contribute to the skin's hydrophobic properties, reducing water loss and enhancing the barrier's effectiveness. A compromised barrier can lead to various skin conditions, including dryness, irritation, and increased susceptibility to infections.
Keratinocytes also play a role in the immune response of the skin. They can produce pro-inflammatory cytokines and antimicrobial peptides in response to injury or infection, helping to recruit immune cells to the site of damage. This ability to respond to environmental threats is crucial for maintaining skin health and preventing disease.
Wound Healing
Keratinocytes are integral to the wound healing process, which involves a series of coordinated events aimed at repairing damaged skin. When the skin is injured, keratinocytes at the wound edges migrate to cover the wound, a process known as re-epithelialization. This migration is facilitated by various growth factors and cytokines released by surrounding cells, including fibroblasts and immune cells.
During wound healing, keratinocytes undergo changes in gene expression that promote their proliferation and migration. They also produce extracellular matrix components that provide structural support for the new tissue. The successful closure of a wound depends on the timely and effective function of keratinocytes, making them a focal point in dermatological research and therapeutic interventions.
In chronic wounds, such as diabetic ulcers or pressure sores, the normal healing process is disrupted, often due to impaired keratinocyte function. Understanding the mechanisms underlying keratinocyte behavior in wound healing can lead to the development of more effective treatments for chronic wounds and skin injuries.
Keratinocyte-Related Skin Disorders
Psoriasis
Psoriasis is a chronic inflammatory skin disorder characterized by the rapid proliferation of keratinocytes, leading to the formation of thick, scaly plaques on the skin. In psoriasis, the normal lifecycle of keratinocytes is accelerated, resulting in a reduced turnover time of approximately 3-5 days instead of the typical 28 days. This rapid turnover leads to the accumulation of immature keratinocytes on the skin's surface, causing the characteristic scaling and inflammation associated with the condition.
The pathogenesis of psoriasis involves a complex interplay between genetic, environmental, and immunological factors. Dysregulation of the immune system plays a significant role in the development of psoriasis, with activated T cells and other immune cells contributing to the inflammatory response. Treatments for psoriasis often target keratinocyte proliferation and inflammation, including topical corticosteroids, systemic medications, and biologic therapies.
Understanding the role of keratinocytes in psoriasis has led to the development of targeted therapies that specifically address the underlying mechanisms of the disease. Research continues to explore the intricate signaling pathways involved in keratinocyte activation and proliferation in psoriasis, aiming to improve treatment outcomes for patients.
Eczema
Eczema, or atopic dermatitis, is a common inflammatory skin condition characterized by dry, itchy, and inflamed skin. Keratinocytes play a crucial role in the pathophysiology of eczema, as they are involved in the skin barrier dysfunction that is a hallmark of the condition. In eczema, the production of lipids and proteins necessary for maintaining the skin barrier is impaired, leading to increased transepidermal water loss and susceptibility to irritants and allergens.
Keratinocytes in eczema exhibit altered gene expression and inflammatory responses, contributing to the chronic inflammation observed in the condition. The interaction between keratinocytes and immune cells, such as T cells and mast cells, further exacerbates the inflammatory response, leading to the characteristic symptoms of eczema.
Management of eczema often involves a multifaceted approach, including the use of emollients to restore the skin barrier, topical corticosteroids to reduce inflammation, and immunomodulatory agents to address the underlying immune dysregulation. Ongoing research aims to better understand the role of keratinocytes in eczema and develop more effective therapies that target the root causes of the condition.
Conclusion
Keratinocytes are fundamental to the structure and function of the skin, playing essential roles in barrier protection, wound healing, and immune response. Their unique biology and the processes they undergo are crucial for maintaining skin health and integrity. Understanding keratinocytes is vital for dermatologists and researchers, as abnormalities in their function can lead to a variety of skin disorders, including psoriasis and eczema.
As research continues to advance our knowledge of keratinocyte biology, new therapeutic strategies are being developed to address skin conditions more effectively. By targeting the underlying mechanisms of keratinocyte dysfunction, it is possible to improve treatment outcomes and enhance the quality of life for individuals affected by skin disorders.
In summary, keratinocytes are not only structural components of the skin but also active participants in various physiological processes. Their importance in dermatology cannot be overstated, as they are central to both the health of the skin and the pathogenesis of numerous skin diseases.
Visit Our Offices
Services:
- • Medical Dermatology
- • Surgical Dermatology
- • Laser Treatments
- • Cosmetic Dermatology
Services:
- • Medical Dermatology
- • Surgical Dermatology
- • Laser Treatments
- • Cosmetic Dermatology
Visit Our Offices
Services:
- • Medical Dermatology
- • Surgical Dermatology
- • Laser Treatments
- • Cosmetic Dermatology
Services:
- • Medical Dermatology
- • Surgical Dermatology
- • Laser Treatments
- • Cosmetic Dermatology