Introduction to Keloids
Keloids are a type of raised scar that occurs when the body produces an excess of collagen during the healing process following an injury to the skin. Unlike normal scars, which typically fade and flatten over time, keloids can continue to grow beyond the original site of injury and may become larger than the wound itself. This abnormal growth can lead to significant physical and psychological implications for those affected, making it essential to understand the nature of keloids, their causes, and available treatment options.
The term "keloid" is derived from the Greek word "cheloides," which means "resembling a tumor." While keloids are not cancerous, their appearance can be distressing, and they may cause discomfort or itching. Keloids can occur on any part of the body but are most commonly found on the chest, shoulders, earlobes, and cheeks. Understanding keloids requires a comprehensive look at their pathophysiology, risk factors, and management strategies.
Pathophysiology of Keloids
The formation of keloids is a complex biological process that involves several stages of wound healing. When the skin is injured, the body initiates a healing response that includes inflammation, tissue formation, and remodeling. In normal wound healing, fibroblasts—cells responsible for collagen production—play a crucial role in forming new tissue. However, in individuals predisposed to keloid formation, this process becomes dysregulated.
In keloid formation, fibroblasts become hyperactive, leading to an overproduction of collagen and other extracellular matrix components. This excessive collagen deposition results in the characteristic raised appearance of keloids. Additionally, the balance between collagen synthesis and degradation is disrupted, with increased levels of collagen type III and decreased levels of collagen type I, contributing to the keloid's unique structure. The exact mechanisms that trigger this abnormal response are still under investigation, but genetic factors, mechanical tension, and certain growth factors are believed to play significant roles.
Genetic Factors
Research has shown that keloids may have a hereditary component, with a higher prevalence among individuals with a family history of keloid formation. Specific genetic markers have been identified that may predispose individuals to develop keloids, suggesting that certain genetic variations can influence the body's healing response. Studies have indicated that mutations in genes involved in collagen synthesis and regulation may contribute to the keloid phenotype.
Mechanical Tension and Growth Factors
Mechanical tension on the skin can also influence keloid formation. Areas of the body that experience more tension during the healing process, such as the chest and shoulders, are more likely to develop keloids. Furthermore, growth factors such as transforming growth factor-beta (TGF-β) and platelet-derived growth factor (PDGF) are implicated in the keloid formation process. These factors stimulate fibroblast proliferation and collagen production, exacerbating the keloid's development.
Risk Factors for Keloid Formation
While anyone can develop keloids, certain risk factors increase the likelihood of their formation. Understanding these risk factors is crucial for prevention and management strategies. The following are some of the most common risk factors associated with keloid development:
- Skin Type: Individuals with darker skin tones, particularly those of African, Asian, or Hispanic descent, are at a higher risk of developing keloids. This increased susceptibility may be related to genetic factors and differences in skin structure.
- Age: Keloids are most commonly seen in individuals aged 10 to 30 years. The increased incidence in this age group may be related to the higher frequency of skin injuries during adolescence and young adulthood.
- Gender: While both males and females can develop keloids, some studies suggest that females may be more prone to keloid formation, possibly due to hormonal influences.
- Previous History: Individuals with a personal history of keloids are at a significantly increased risk of developing new keloids, especially after surgical procedures or skin trauma.
Common Causes of Keloids
Keloids can arise from various types of skin injuries, including surgical incisions, cuts, burns, insect bites, and even acne lesions. Understanding the common causes of keloids can help individuals take preventive measures to minimize their risk. Some of the most frequent causes include:
- Surgical Scars: Surgical procedures, particularly those involving the chest and shoulders, are among the most common causes of keloids. The tension and trauma associated with surgery can trigger an abnormal healing response.
- Trauma: Any form of skin trauma, including cuts, abrasions, or injuries, can lead to keloid formation. Even minor injuries that may not typically result in scarring can cause keloids in susceptible individuals.
- Body Piercings: Keloids frequently occur at the site of body piercings, particularly in individuals with a predisposition to keloid formation. The inflammation and healing process associated with piercings can trigger excessive collagen production.
- Acne: Severe acne can lead to scarring, and in some cases, keloids may form at the site of acne lesions. This is particularly true for individuals with a history of keloid formation.
Symptoms and Diagnosis of Keloids
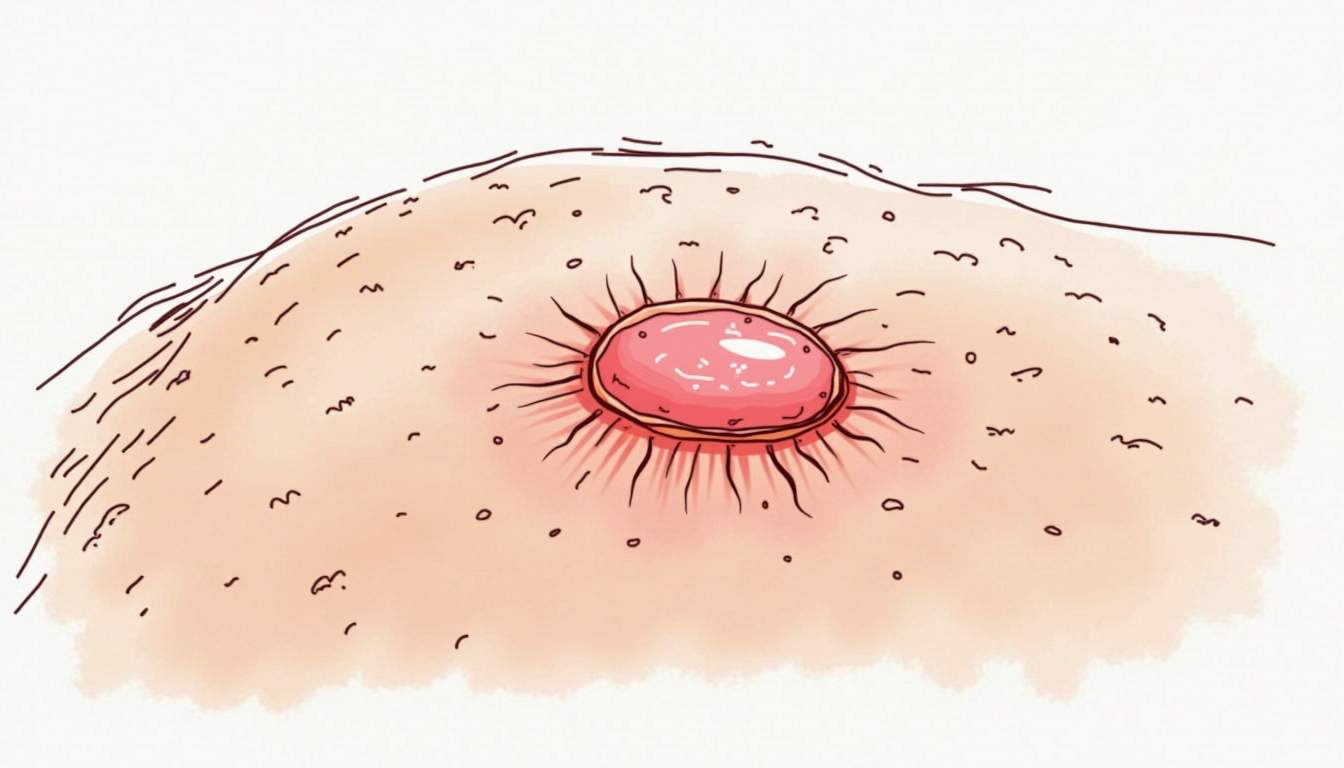
Keloids are characterized by their distinct appearance and can present with various symptoms. The most common symptoms associated with keloids include:
- Raised Appearance: Keloids are typically raised above the surrounding skin and can vary in size from small to large. They may continue to grow over time, often extending beyond the original injury site.
- Color Changes: Keloids may appear red, purple, or darker than the surrounding skin, especially in individuals with darker skin tones. Over time, they may become lighter but often remain raised.
- Itching or Pain: Some individuals may experience itching, tenderness, or pain at the keloid site. These sensations can vary in intensity and may be more pronounced during periods of stress or skin irritation.
Diagnosis of keloids is primarily clinical and involves a thorough examination of the lesion and the patient's medical history. Dermatologists may ask about the patient's history of skin injuries, family history of keloids, and any previous treatments. In some cases, a biopsy may be performed to rule out other skin conditions that may mimic keloids.
Treatment Options for Keloids
Managing keloids can be challenging, and treatment options vary depending on the size, location, and symptoms of the keloid, as well as the patient's preferences. While complete removal of keloids is often difficult, several treatment modalities can help reduce their size and improve their appearance. The following are some of the most commonly used treatment options:
1. Corticosteroid Injections
Corticosteroid injections are one of the most common treatments for keloids. These injections help to reduce inflammation and collagen production, leading to a decrease in the size and thickness of the keloid. Patients typically receive multiple injections over several weeks or months, and while this treatment can be effective, it may require ongoing maintenance to prevent recurrence.
2. Surgical Excision
Surgical excision involves the complete removal of the keloid. While this method can provide immediate results, there is a risk of recurrence, and in some cases, the new scar may develop into another keloid. To minimize the risk of recurrence, surgeons may combine excision with other treatments, such as corticosteroid injections or radiation therapy.
3. Cryotherapy
Cryotherapy involves freezing the keloid with liquid nitrogen, which can help to reduce its size. This treatment is often used in combination with other therapies, such as corticosteroid injections, to enhance its effectiveness. Cryotherapy is particularly useful for smaller keloids and may require multiple sessions for optimal results.
4. Silicone Gel Sheets
Silicone gel sheets are a non-invasive treatment option that can help flatten and soften keloids over time. These sheets are applied directly to the keloid and worn for several hours each day. While silicone gel sheets may not completely eliminate keloids, they can significantly improve their appearance and reduce symptoms such as itching.
5. Radiation Therapy
Radiation therapy is sometimes used as an adjunct treatment following surgical excision to reduce the risk of keloid recurrence. Low-dose radiation can help inhibit fibroblast activity and collagen production, making it a valuable option for patients with a history of keloid formation. However, the use of radiation therapy requires careful consideration of potential long-term risks.
Prevention of Keloids
Preventing keloids can be particularly challenging, especially for individuals with a history of keloid formation. However, there are several strategies that may help reduce the risk of developing keloids:
- Avoiding Unnecessary Skin Trauma: Minimizing skin injuries, such as cuts and abrasions, can help reduce the risk of keloid formation. Individuals prone to keloids should be cautious during activities that may lead to skin trauma.
- Careful Management of Surgical Scars: For individuals undergoing surgery, discussing keloid prevention strategies with the surgeon is essential. Techniques such as tension-free closure and the use of silicone gel sheets post-surgery may help minimize the risk of keloid formation.
- Prompt Treatment of Skin Injuries: Treating skin injuries promptly and effectively can help reduce the risk of keloids. Keeping wounds clean and covered, and seeking medical attention for more severe injuries, can promote proper healing.
- Consultation with a Dermatologist: Individuals with a history of keloids should consult with a dermatologist for personalized prevention strategies and treatment options. Early intervention can be crucial in managing keloid formation.
Conclusion
Keloids represent a unique and often distressing dermatological condition that can significantly impact an individual's quality of life. Understanding the underlying mechanisms, risk factors, and treatment options is essential for effective management. While complete prevention of keloids may not be possible for everyone, awareness and proactive measures can help reduce the likelihood of their formation. For those affected, a multidisciplinary approach involving dermatologists, plastic surgeons, and other healthcare professionals can provide the best outcomes in managing keloids and improving overall skin health.
Visit Our Offices
Services:
- • Medical Dermatology
- • Surgical Dermatology
- • Laser Treatments
- • Cosmetic Dermatology
Services:
- • Medical Dermatology
- • Surgical Dermatology
- • Laser Treatments
- • Cosmetic Dermatology
Visit Our Offices
Services:
- • Medical Dermatology
- • Surgical Dermatology
- • Laser Treatments
- • Cosmetic Dermatology
Services:
- • Medical Dermatology
- • Surgical Dermatology
- • Laser Treatments
- • Cosmetic Dermatology