Definition of Intertrigo
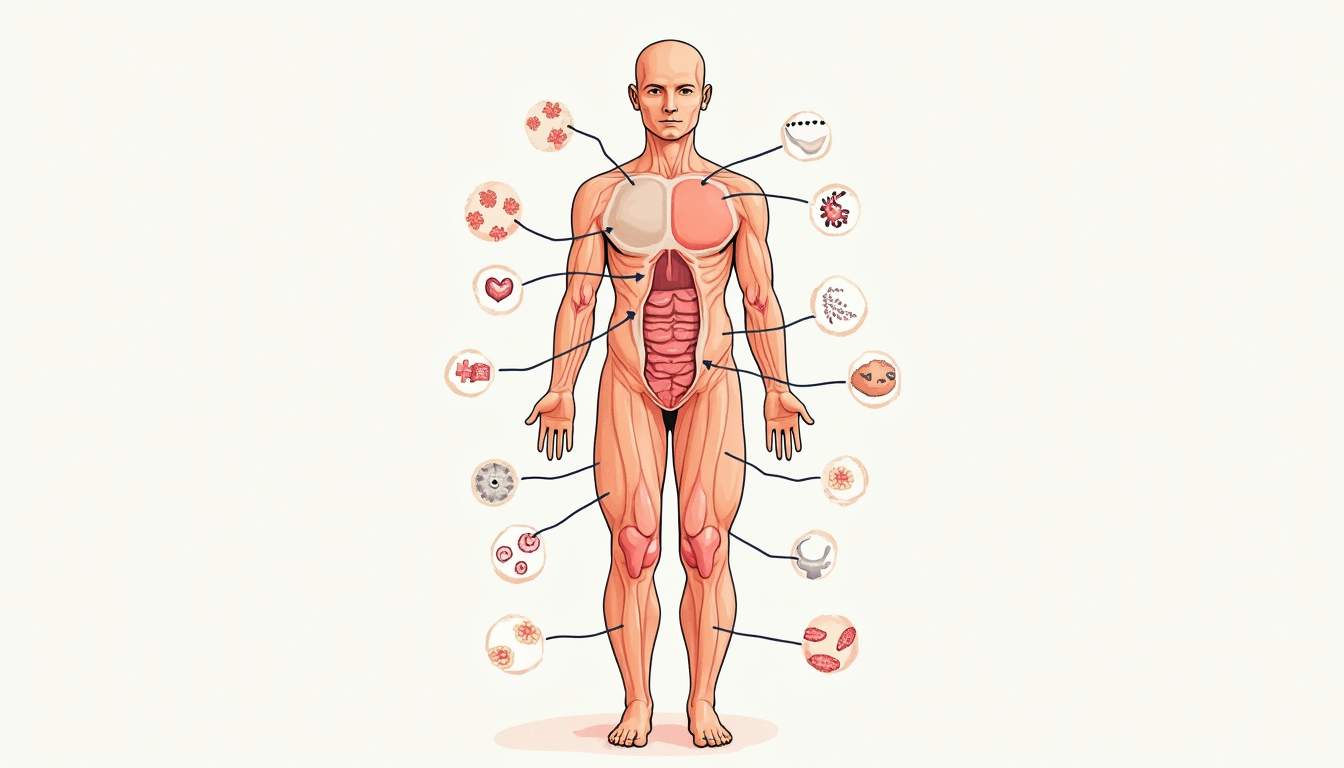
Intertrigo is a common inflammatory skin condition that occurs in skin folds where two surfaces rub against each other. It is characterized by redness, irritation, and sometimes the presence of a secondary infection. The condition is often exacerbated by moisture, heat, and friction, making it prevalent in areas such as the armpits, groin, under the breasts, and between the toes. Intertrigo is not a disease in itself but rather a manifestation of skin irritation due to various factors, including skin-on-skin friction and the presence of sweat.
The term "intertrigo" is derived from the Latin words "inter," meaning between, and "trigo," meaning to rub. This etymology aptly describes the condition's nature, as it arises in areas where skin surfaces are in constant contact. While intertrigo can affect individuals of all ages, it is particularly common in obese individuals, infants, and the elderly, who may have more pronounced skin folds.
Understanding intertrigo is crucial for dermatologists and healthcare providers, as it can lead to significant discomfort and may predispose individuals to secondary infections, such as candidiasis or bacterial infections. Effective management involves identifying the underlying causes, implementing preventive measures, and providing appropriate treatment to alleviate symptoms.
Causes of Intertrigo
Friction and Moisture
The primary causes of intertrigo are friction and moisture. When skin surfaces rub against each other, it can lead to irritation and inflammation. This friction is often exacerbated by factors such as obesity, which increases the number of skin folds, and physical activity, which can lead to sweating. Moisture from sweat or other sources can further irritate the skin, creating an environment conducive to inflammation.
In addition to natural moisture from sweat, intertrigo can also be aggravated by external factors such as occlusive clothing or the use of heavy creams and ointments that trap moisture in the skin folds. This combination of friction and moisture creates a perfect storm for irritation, leading to the characteristic symptoms of intertrigo.
Furthermore, certain activities that involve repetitive movements, such as running or cycling, can increase the likelihood of developing intertrigo due to the constant friction and moisture in the affected areas. Understanding these causes is essential for both prevention and treatment.
Underlying Medical Conditions
Several underlying medical conditions can contribute to the development of intertrigo. Conditions that lead to increased sweating, such as hyperhidrosis, can make individuals more susceptible to intertrigo. Additionally, skin conditions like eczema or psoriasis may predispose individuals to skin irritation and inflammation in skin folds.
Diabetes is another condition that can increase the risk of intertrigo. Individuals with diabetes may experience changes in skin integrity and increased susceptibility to infections, making them more vulnerable to developing intertrigo. Similarly, immunocompromised individuals, such as those undergoing chemotherapy or living with HIV/AIDS, may have a higher risk due to their compromised skin barrier and immune response.
Recognizing these underlying conditions is crucial for healthcare providers, as addressing them can significantly impact the management and prevention of intertrigo.
Symptoms of Intertrigo
Clinical Presentation
The clinical presentation of intertrigo typically includes redness, swelling, and irritation in the affected skin folds. Patients may report symptoms such as itching, burning, or stinging sensations in the affected areas. The skin may appear shiny and may have a moist or weepy appearance due to the accumulation of sweat and other secretions.
In some cases, intertrigo can progress to involve secondary infections, which may manifest as pustules, crusting, or the presence of a foul odor. These secondary infections can complicate the clinical picture and may require additional treatment. It is essential for healthcare providers to differentiate between simple intertrigo and intertrigo complicated by infections, as the management strategies may differ significantly.
In infants, intertrigo may present as a bright red rash in the diaper area or in skin folds, often accompanied by satellite lesions caused by yeast infections. This presentation can be particularly distressing for caregivers and may require prompt intervention.
Complications
While intertrigo itself is not a serious condition, it can lead to complications if not managed appropriately. One of the most common complications is the development of secondary infections, particularly fungal infections caused by Candida species. These infections can lead to more severe symptoms, including increased pain, swelling, and the formation of pustules.
Bacterial infections, such as those caused by Staphylococcus aureus, can also occur, particularly in cases where the skin barrier is compromised. These infections may require systemic antibiotics and can lead to further complications if left untreated.
In chronic cases, intertrigo can lead to skin thickening and changes in pigmentation, which may be cosmetically concerning for patients. Therefore, early recognition and management of intertrigo are essential to prevent these complications.
Diagnosis of Intertrigo
Clinical Evaluation
The diagnosis of intertrigo is primarily clinical and involves a thorough evaluation of the patient's history and physical examination. Healthcare providers will assess the affected areas for characteristic signs of intertrigo, including redness, irritation, and the presence of any secondary infections.
During the evaluation, it is essential to obtain a detailed history, including any underlying medical conditions, medications, and lifestyle factors that may contribute to the development of intertrigo. This information can help guide treatment decisions and preventive measures.
In some cases, additional diagnostic tests may be warranted to rule out other conditions that may mimic intertrigo, such as contact dermatitis or other inflammatory skin conditions. These tests may include skin scrapings to check for fungal infections or patch testing to identify potential allergens.
Differential Diagnosis
Several conditions may present similarly to intertrigo, making a differential diagnosis essential. Conditions such as contact dermatitis, which can occur due to irritants or allergens, may present with similar symptoms of redness and irritation in skin folds. Psoriasis, with its characteristic plaques and scaling, can also be confused with intertrigo, particularly in areas of friction.
Other conditions to consider include candidiasis, which often presents with a bright red rash and satellite lesions, and bacterial infections, which may present with pustules or crusting. A thorough clinical evaluation and, if necessary, laboratory testing can help differentiate these conditions and guide appropriate management.
In summary, accurate diagnosis is crucial for effective treatment, and healthcare providers must consider the full spectrum of potential differential diagnoses when evaluating a patient with suspected intertrigo.
Treatment of Intertrigo
General Management Strategies
The management of intertrigo focuses on alleviating symptoms, preventing recurrence, and addressing any underlying causes. General strategies include keeping the affected areas clean and dry, minimizing friction, and avoiding irritants. Patients are often advised to use gentle cleansers and to pat the skin dry rather than rubbing it.
In cases where moisture is a significant contributing factor, the use of absorbent powders or barrier creams may be beneficial. These products can help reduce friction and absorb excess moisture, creating a more favorable environment for healing. Patients should be educated on the importance of maintaining skin integrity and avoiding tight clothing that may exacerbate friction.
For patients with underlying medical conditions, managing those conditions is crucial. For instance, individuals with diabetes should work to control their blood sugar levels, as this can impact skin health and susceptibility to infections. Similarly, addressing obesity through lifestyle modifications may help reduce the number of skin folds and the risk of intertrigo.
Topical Treatments
Topical treatments play a significant role in the management of intertrigo. For mild cases, over-the-counter antifungal powders or creams may be effective in reducing inflammation and preventing secondary infections. Commonly used antifungal agents include clotrimazole and miconazole, which can help address any underlying fungal component of the condition.
In cases where inflammation is more pronounced, topical corticosteroids may be prescribed to reduce redness and swelling. However, caution should be exercised when using corticosteroids in intertrigo, as prolonged use can lead to skin thinning and other complications. It is essential to follow the healthcare provider's recommendations regarding the use of these medications.
For patients with secondary bacterial infections, topical antibiotics may be necessary. Healthcare providers may prescribe agents such as mupirocin or fusidic acid to target the specific bacteria involved. In more severe cases, systemic antibiotics may be required to address widespread infections.
Prevention of Intertrigo
Personal Hygiene Practices
Preventing intertrigo involves implementing effective personal hygiene practices. Keeping the skin clean and dry is paramount, particularly in areas prone to friction and moisture. Regular bathing with mild soap can help remove sweat and debris, while thorough drying of skin folds is essential to prevent moisture accumulation.
For individuals at higher risk, such as those with obesity or diabetes, additional preventive measures may be necessary. Wearing loose-fitting clothing made from breathable fabrics can help reduce friction and allow for better air circulation. Additionally, using moisture-wicking fabrics during physical activity can help keep the skin dry and reduce the risk of intertrigo.
Regular skin assessments are also important, particularly for individuals with underlying medical conditions. Early recognition of any signs of irritation can lead to prompt intervention and prevent the progression of intertrigo.
Weight Management and Lifestyle Modifications
For individuals with obesity, weight management is a critical component of intertrigo prevention. Reducing body weight can decrease the number of skin folds and the associated friction and moisture. Engaging in regular physical activity, combined with a balanced diet, can help achieve and maintain a healthy weight.
In addition to weight management, lifestyle modifications such as smoking cessation and stress management can also play a role in skin health. Smoking can impair circulation and wound healing, while stress can exacerbate skin conditions. By addressing these factors, individuals can improve their overall skin health and reduce the risk of intertrigo.
Ultimately, a comprehensive approach to prevention that includes personal hygiene practices, weight management, and lifestyle modifications can significantly reduce the incidence of intertrigo and improve the quality of life for affected individuals.
Conclusion
Intertrigo is a common yet often overlooked skin condition that can cause significant discomfort and complications if not managed appropriately. Understanding the causes, symptoms, diagnosis, and treatment options is essential for healthcare providers and patients alike. By implementing effective preventive measures and addressing underlying medical conditions, individuals can reduce their risk of developing intertrigo and improve their overall skin health.
As with many dermatological conditions, early recognition and intervention are key to successful management. Patients should be encouraged to seek medical advice if they experience symptoms of intertrigo, particularly if they notice signs of secondary infections. With appropriate care and attention, intertrigo can be effectively managed, allowing individuals to lead comfortable and healthy lives.
Visit Our Offices
Services:
- • Medical Dermatology
- • Surgical Dermatology
- • Laser Treatments
- • Cosmetic Dermatology
Services:
- • Medical Dermatology
- • Surgical Dermatology
- • Laser Treatments
- • Cosmetic Dermatology
Visit Our Offices
Services:
- • Medical Dermatology
- • Surgical Dermatology
- • Laser Treatments
- • Cosmetic Dermatology
Services:
- • Medical Dermatology
- • Surgical Dermatology
- • Laser Treatments
- • Cosmetic Dermatology