Understanding the Immune Response
The immune response is a complex biological process that protects the body from harmful pathogens, including bacteria, viruses, fungi, and parasites. It involves a sophisticated network of cells, tissues, and organs that work together to identify and eliminate these threats. In dermatology, the immune response plays a crucial role in skin health and disease, influencing conditions such as eczema, psoriasis, and skin infections.
The immune system is generally divided into two main components: the innate immune system and the adaptive immune system. The innate immune system is the body's first line of defense, providing immediate but non-specific responses to pathogens. In contrast, the adaptive immune system develops a targeted response to specific pathogens, creating immunological memory that allows for a quicker response upon subsequent exposures.
In the context of dermatology, understanding the immune response is essential for diagnosing and treating various skin conditions. The skin acts as a physical barrier, but when this barrier is compromised, the immune system is activated, leading to inflammation and other immune-mediated reactions that can manifest as skin disorders.
The Role of Skin in Immune Defense
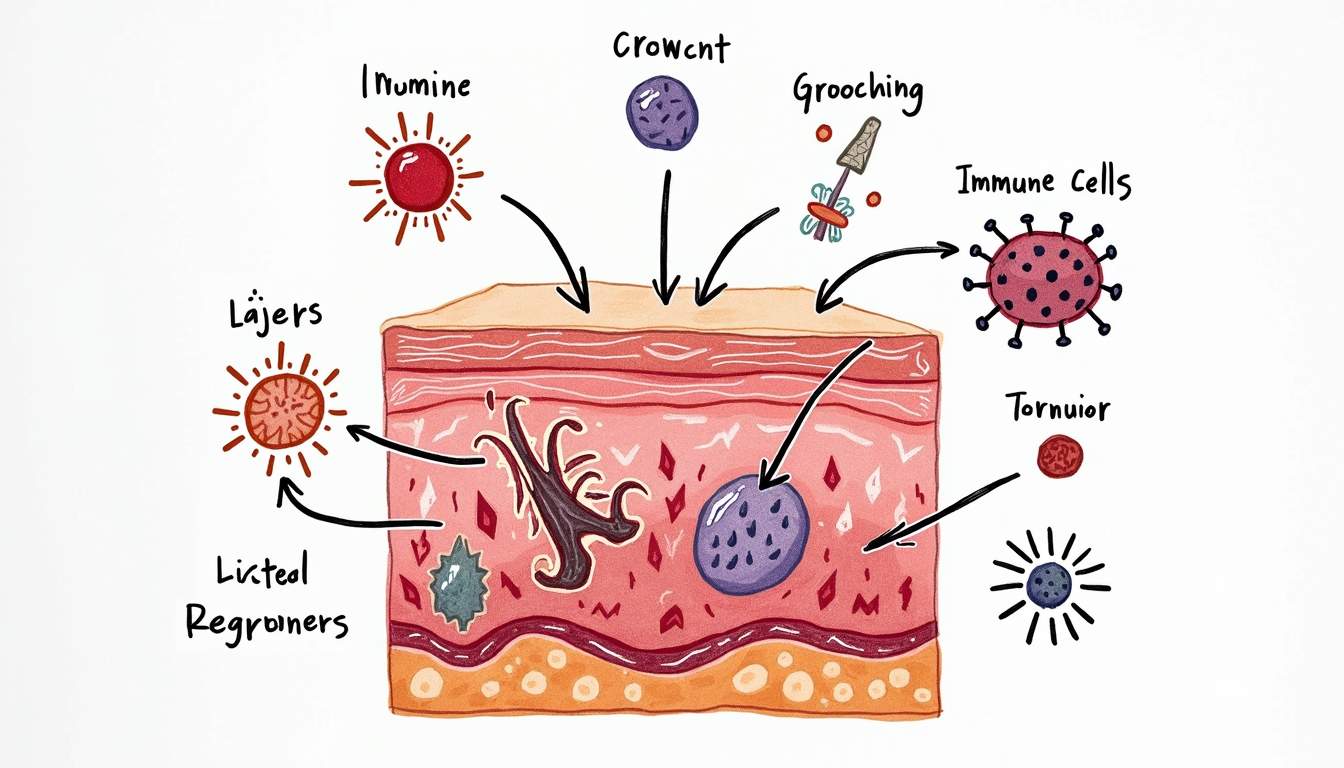
The skin is not merely a protective covering; it is an active participant in the immune response. Composed of multiple layers, including the epidermis, dermis, and subcutaneous tissue, the skin contains various immune cells that play critical roles in defending against infections. Keratinocytes, the primary cells of the epidermis, produce antimicrobial peptides and cytokines that help initiate the immune response.
Additionally, specialized immune cells such as Langerhans cells, a type of dendritic cell found in the epidermis, are crucial for antigen presentation. These cells capture and process pathogens, presenting their antigens to T cells in the lymph nodes, thereby bridging the innate and adaptive immune responses. The dermis also contains other immune cells, such as macrophages and mast cells, which further contribute to the skin's immune defense.
Moreover, the skin's microbiome, which consists of a diverse community of microorganisms, plays a significant role in modulating the immune response. A balanced skin microbiome can enhance the skin's barrier function and promote a healthy immune response, while dysbiosis can lead to inflammatory skin conditions.
Types of Immune Responses in Dermatology
Innate Immune Response
The innate immune response is the body's first line of defense against pathogens. It is characterized by immediate action and includes physical barriers, such as the skin and mucous membranes, as well as immune cells that respond quickly to infections. In dermatology, the innate immune response is crucial for preventing skin infections and controlling inflammation.
Key components of the innate immune response in the skin include:
- Keratinocytes: These cells produce antimicrobial peptides and cytokines that help to fight off infections.
- Langerhans Cells: These dendritic cells capture and present antigens to T cells, initiating the adaptive immune response.
- Mast Cells: These cells release histamine and other mediators during allergic reactions and contribute to inflammation.
- Macrophages: These phagocytic cells engulf pathogens and dead cells, playing a vital role in tissue repair and inflammation.
Adaptive Immune Response
The adaptive immune response is characterized by its specificity and memory. It takes longer to develop than the innate response but provides a more targeted and effective defense against specific pathogens. In dermatology, the adaptive immune response is particularly relevant in chronic skin conditions such as psoriasis and atopic dermatitis.
Key features of the adaptive immune response include:
- B Cells: These cells produce antibodies that specifically target antigens, neutralizing pathogens and marking them for destruction.
- T Cells: There are several types of T cells, including helper T cells (CD4+) that assist other immune cells and cytotoxic T cells (CD8+) that directly kill infected cells.
- Memory Cells: After an initial infection, some B and T cells become memory cells, allowing for a quicker and more robust response upon re-exposure to the same pathogen.
Inflammation and Its Role in Skin Disorders
Inflammation is a key component of the immune response and plays a crucial role in dermatological conditions. It is a protective mechanism that helps the body fight infections and heal injuries. However, when inflammation becomes chronic, it can lead to various skin disorders, including eczema, psoriasis, and acne.
In the skin, inflammation is characterized by redness, swelling, heat, and pain. These symptoms arise from the increased blood flow to the affected area and the accumulation of immune cells. Inflammatory cytokines, such as interleukins and tumor necrosis factor-alpha (TNF-alpha), are released by immune cells and contribute to the inflammatory process.
Chronic inflammation in the skin can result from various factors, including persistent infections, autoimmune reactions, and environmental triggers. Understanding the mechanisms of inflammation is essential for developing effective treatments for inflammatory skin conditions.
Common Dermatological Conditions Related to Immune Response
Atopic Dermatitis
Atopic dermatitis, commonly known as eczema, is a chronic inflammatory skin condition characterized by dry, itchy, and inflamed skin. It is believed to result from a combination of genetic predisposition, environmental factors, and immune dysregulation. The immune response in atopic dermatitis is marked by an overactive Th2 (T-helper 2) response, leading to increased levels of IgE antibodies and elevated levels of inflammatory cytokines.
Patients with atopic dermatitis often have a compromised skin barrier, making them more susceptible to allergens and irritants. This condition is frequently associated with other allergic diseases, such as asthma and allergic rhinitis, highlighting the interconnectedness of the immune system in various allergic responses.
Psoriasis
Psoriasis is a chronic autoimmune skin disorder characterized by the rapid proliferation of skin cells, leading to thick, scaly plaques. The immune response in psoriasis involves an overactive Th1 and Th17 response, resulting in the release of pro-inflammatory cytokines that drive the hyperproliferation of keratinocytes. This condition is often associated with systemic inflammation and can have significant impacts on a patient's quality of life.
Understanding the immune mechanisms underlying psoriasis has led to the development of targeted therapies, including biologics that specifically inhibit cytokines involved in the inflammatory process. These treatments aim to restore immune balance and improve skin health.
Acne Vulgaris
Acne vulgaris is a common skin condition characterized by the presence of comedones, papules, pustules, and sometimes cysts. It is primarily caused by the overproduction of sebum, clogged hair follicles, and the proliferation of the bacterium Propionibacterium acnes. The immune response plays a significant role in the pathogenesis of acne, as the presence of P. acnes triggers an inflammatory response that contributes to the formation of acne lesions.
Inflammation in acne is mediated by the release of cytokines and chemokines that attract immune cells to the site of infection. This inflammatory response can exacerbate the severity of acne and lead to scarring. Treatments for acne often focus on reducing inflammation, controlling sebum production, and targeting P. acnes.
Therapeutic Approaches Targeting the Immune Response
Understanding the immune response in dermatology has paved the way for innovative therapeutic approaches aimed at modulating immune function. These treatments can be broadly categorized into topical therapies, systemic medications, and biologic agents.
Topical Therapies
Topical therapies are often the first line of treatment for various dermatological conditions. These include corticosteroids, calcineurin inhibitors, and retinoids, which work by reducing inflammation, modulating immune responses, and promoting skin cell turnover. Corticosteroids, for example, are potent anti-inflammatory agents that can effectively manage conditions like eczema and psoriasis by suppressing the immune response in the affected area.
Calcineurin inhibitors, such as tacrolimus and pimecrolimus, are non-steroidal options that inhibit T-cell activation and are particularly useful for sensitive areas of the skin. Retinoids, derived from vitamin A, help normalize skin cell differentiation and reduce inflammation, making them effective for acne and psoriasis.
Systemic Medications
For more severe or refractory skin conditions, systemic medications may be necessary. These include oral corticosteroids, immunosuppressants, and systemic retinoids. Oral corticosteroids can provide rapid relief from inflammation but are generally used for short durations due to potential side effects.
Immunosuppressants, such as methotrexate and azathioprine, work by inhibiting the proliferation of immune cells and are often used for chronic conditions like psoriasis. Systemic retinoids, such as isotretinoin, are effective for severe acne by targeting multiple factors, including sebum production and inflammation.
Biologic Agents
Biologic agents represent a breakthrough in the treatment of immune-mediated skin disorders. These medications are designed to target specific components of the immune system, such as cytokines or immune cell receptors. For instance, monoclonal antibodies that inhibit TNF-alpha, IL-17, or IL-23 have shown remarkable efficacy in treating psoriasis and other inflammatory skin conditions.
Biologics offer the advantage of a targeted approach, reducing the risk of systemic side effects associated with traditional immunosuppressive therapies. However, they require careful patient selection and monitoring due to potential risks, including infections and malignancies.
Conclusion
The immune response is a fundamental aspect of dermatology, influencing the pathogenesis, presentation, and treatment of various skin conditions. A comprehensive understanding of the immune system's role in skin health is essential for dermatologists and healthcare providers to effectively manage and treat patients with dermatological disorders.
As research continues to unveil the complexities of the immune response in the skin, new therapeutic strategies will emerge, offering hope for improved outcomes for patients suffering from chronic and inflammatory skin conditions. The interplay between the immune system and dermatological health underscores the importance of an integrated approach to skin care, emphasizing the need for ongoing education and collaboration among healthcare professionals.
Visit Our Offices
Services:
- • Medical Dermatology
- • Surgical Dermatology
- • Laser Treatments
- • Cosmetic Dermatology
Services:
- • Medical Dermatology
- • Surgical Dermatology
- • Laser Treatments
- • Cosmetic Dermatology
Visit Our Offices
Services:
- • Medical Dermatology
- • Surgical Dermatology
- • Laser Treatments
- • Cosmetic Dermatology
Services:
- • Medical Dermatology
- • Surgical Dermatology
- • Laser Treatments
- • Cosmetic Dermatology