Definition of Hyperkeratosis
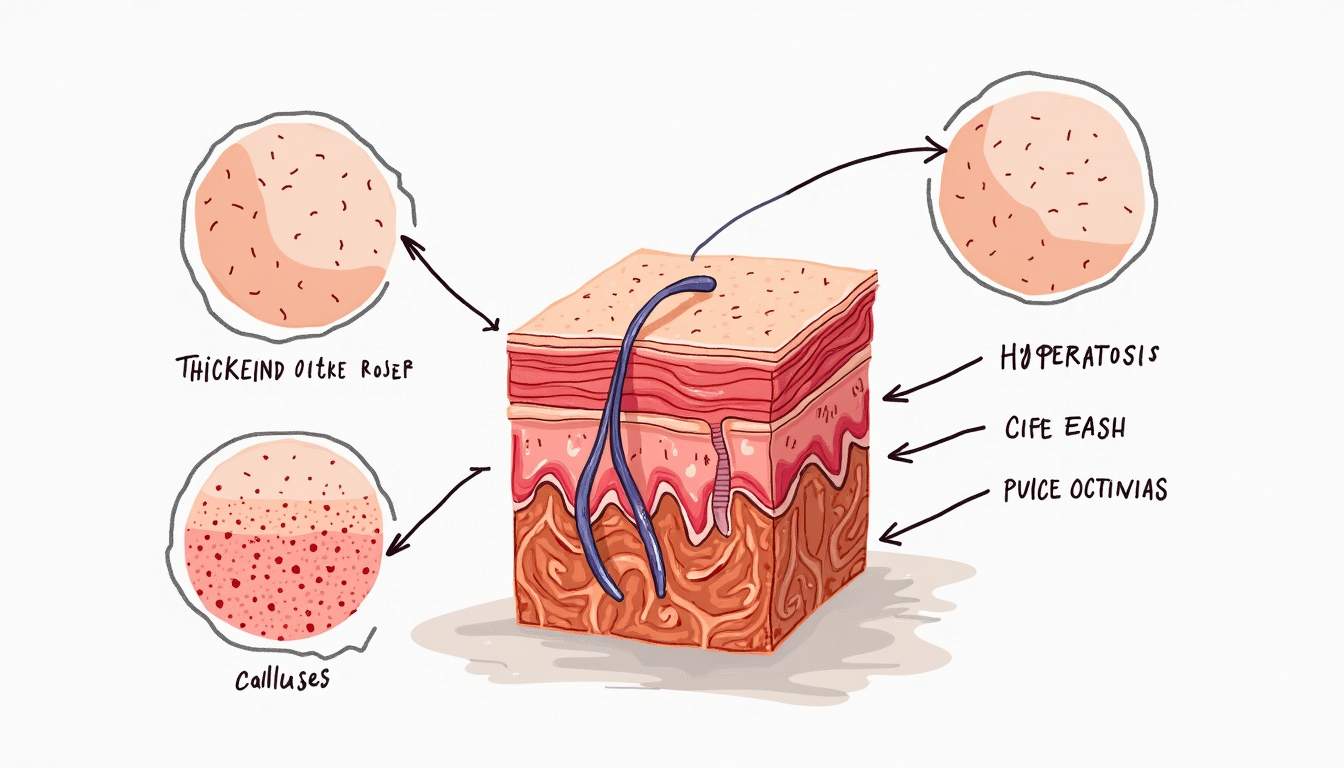
Hyperkeratosis is a dermatological condition characterized by the thickening of the outer layer of the skin, known as the stratum corneum. This thickening occurs due to an increase in the production of keratin, a fibrous protein that is a key structural component of the skin, hair, and nails. The condition can manifest in various forms and can be localized or generalized, depending on the underlying cause.
The term "hyperkeratosis" is derived from the Greek words "hyper," meaning excessive, and "keratosis," referring to the formation of keratin. This condition can be a response to various stimuli, including chronic friction, pressure, or irritation, and can also be associated with certain diseases or genetic disorders.
Understanding hyperkeratosis is crucial for dermatologists and healthcare professionals as it can serve as a clinical indicator of underlying health issues. The condition can present in a variety of forms, each with its own specific characteristics and implications for treatment.
Types of Hyperkeratosis
Hyperkeratosis can be classified into several types based on its appearance, location, and underlying causes. Each type presents unique challenges for diagnosis and treatment. Below are some of the most common types of hyperkeratosis:
1. Actinic Keratosis
Actinic keratosis (AK) is a precancerous condition that arises from prolonged sun exposure. It typically appears as rough, scaly patches on sun-exposed areas of the skin, such as the face, ears, and hands. AK is characterized by a thickened, crusty surface and may be accompanied by redness or inflammation. Individuals with fair skin are at a higher risk of developing AK, and it is essential to monitor these lesions for any changes that could indicate progression to skin cancer.
Actinic keratosis is often treated with topical medications, cryotherapy, or photodynamic therapy. Regular skin examinations by a dermatologist are recommended for early detection and management of AK.
2. Psoriasis
Psoriasis is a chronic autoimmune condition that leads to the rapid proliferation of skin cells, resulting in thick, red, scaly patches on the skin. Hyperkeratosis is a prominent feature of psoriasis, particularly in the form of plaques that can be itchy and painful. The condition can affect any part of the body, but it is most commonly seen on the elbows, knees, scalp, and lower back.
Treatment for psoriasis may include topical corticosteroids, vitamin D analogs, and systemic therapies, depending on the severity of the disease. Lifestyle modifications, such as stress management and dietary changes, can also play a role in managing symptoms.
3. Keratosis Pilaris
Keratosis pilaris is a common, benign skin condition characterized by the appearance of small, rough bumps on the skin, often resembling gooseflesh. These bumps are caused by the accumulation of keratin around hair follicles, leading to localized hyperkeratosis. Keratosis pilaris commonly occurs on the upper arms, thighs, and cheeks and is often more noticeable during dry weather.
While keratosis pilaris is harmless and typically does not require treatment, individuals may seek cosmetic interventions to improve the skin's appearance. Exfoliating creams and moisturizers containing urea or alpha hydroxy acids can help reduce the rough texture.
4. Plantar Keratosis
Plantar keratosis, also known as plantar warts or calluses, occurs on the soles of the feet and is often a response to repeated friction or pressure. This type of hyperkeratosis can be painful and may interfere with walking or standing. Plantar keratosis can develop in individuals who frequently wear ill-fitting shoes or engage in activities that put excessive pressure on the feet.
Treatment options for plantar keratosis include the use of orthotic devices, padding, and topical treatments to soften the thickened skin. In some cases, cryotherapy or surgical removal may be necessary for persistent lesions.
Causes of Hyperkeratosis
The causes of hyperkeratosis can be multifactorial, ranging from environmental factors to genetic predispositions. Understanding these causes is essential for effective management and treatment of the condition. Below are some of the primary causes of hyperkeratosis:
1. Chronic Friction and Pressure
One of the most common causes of hyperkeratosis is chronic friction or pressure on the skin. This can occur in areas where the skin is subjected to repeated rubbing or irritation, such as the hands, feet, and elbows. Occupational factors, such as manual labor or sports activities, can contribute to the development of localized hyperkeratosis.
In these cases, the body responds to the mechanical stress by increasing keratin production, leading to thickened skin as a protective mechanism. Reducing friction through proper footwear, protective gear, and ergonomic adjustments can help alleviate symptoms.
2. Genetic Factors
Some forms of hyperkeratosis have a genetic basis, with certain hereditary conditions leading to abnormal keratinization. For example, conditions such as ichthyosis and epidermolytic hyperkeratosis are characterized by excessive keratin production and thickened skin. These genetic disorders often require specialized care and management strategies tailored to the individual's needs.
Genetic counseling may be beneficial for individuals with a family history of hyperkeratosis or related skin conditions, as it can provide insights into the likelihood of inheritance and potential management options.
3. Environmental Factors
Environmental factors, such as exposure to harsh chemicals, irritants, or extreme weather conditions, can also contribute to hyperkeratosis. For instance, individuals who work in industries involving frequent exposure to solvents or abrasive materials may develop thickened skin as a protective response.
Additionally, climatic conditions such as low humidity can exacerbate dry skin, leading to increased keratin production. Implementing protective measures, such as wearing gloves or using emollients, can help mitigate the effects of environmental factors on the skin.
Diagnosis of Hyperkeratosis
Diagnosing hyperkeratosis involves a thorough clinical evaluation by a dermatologist, who will assess the patient's medical history, symptoms, and physical examination findings. The following steps are typically involved in the diagnostic process:
1. Medical History
The dermatologist will begin by taking a comprehensive medical history, including information about the patient's skin condition, duration of symptoms, and any previous treatments. Family history of skin disorders may also be relevant, as certain types of hyperkeratosis can have a genetic component.
Additionally, the dermatologist may inquire about lifestyle factors, such as occupational exposures, sun protection practices, and skincare routines, to identify potential contributing factors to the condition.
2. Physical Examination
A detailed physical examination of the affected areas will be conducted to assess the characteristics of the hyperkeratosis. The dermatologist will evaluate the texture, color, and distribution of the lesions, as well as any associated symptoms such as itching or pain.
In some cases, a skin biopsy may be performed to obtain a sample of the affected skin for histopathological examination. This can help differentiate hyperkeratosis from other skin conditions and guide appropriate treatment strategies.
Treatment Options for Hyperkeratosis
Treatment for hyperkeratosis depends on the underlying cause, severity of the condition, and the specific type of hyperkeratosis diagnosed. A variety of treatment modalities are available, ranging from topical therapies to procedural interventions. Below are some common treatment options:
1. Topical Treatments
Topical treatments are often the first line of defense in managing hyperkeratosis. These may include:
- Keratinolytic Agents: Products containing urea, salicylic acid, or alpha hydroxy acids help to soften and exfoliate thickened skin, promoting the shedding of excess keratin.
- Corticosteroids: Topical corticosteroids can reduce inflammation and itching associated with certain types of hyperkeratosis, such as psoriasis.
- Moisturizers: Regular use of emollients can help maintain skin hydration and prevent further thickening of the skin.
2. Procedural Interventions
In cases where topical treatments are insufficient, procedural interventions may be considered. These can include:
- Cryotherapy: This involves freezing the affected skin with liquid nitrogen, leading to the destruction of hyperkeratotic tissue.
- Laser Therapy: Certain laser treatments can target and remove thickened skin while promoting healthy skin regeneration.
- Electrosurgery: This technique uses electrical currents to remove hyperkeratotic lesions effectively.
Prevention of Hyperkeratosis
Preventing hyperkeratosis involves adopting healthy skincare practices and minimizing exposure to known risk factors. Below are some strategies to help prevent the development of hyperkeratosis:
1. Sun Protection
Since actinic keratosis is primarily caused by sun exposure, protecting the skin from ultraviolet (UV) radiation is crucial. This can be achieved by:
- Wearing broad-spectrum sunscreen with an SPF of 30 or higher.
- Donning protective clothing, such as hats and long sleeves, when outdoors.
- Avoiding sun exposure during peak hours (10 a.m. to 4 p.m.).
2. Proper Footwear
To prevent plantar keratosis, it is essential to wear well-fitting shoes that provide adequate support and cushioning. Avoiding high heels and tight footwear can help reduce pressure on the feet, minimizing the risk of developing calluses and warts.
3. Skin Care Routine
Establishing a consistent skincare routine that includes regular exfoliation and moisturizing can help maintain skin health and prevent hyperkeratosis. Using gentle exfoliating products and hydrating creams can promote the shedding of dead skin cells and keep the skin barrier intact.
Conclusion
Hyperkeratosis is a common dermatological condition that can arise from various causes, including chronic friction, genetic factors, and environmental influences. Understanding the different types of hyperkeratosis, their causes, and treatment options is essential for effective management. By adopting preventive measures and seeking timely medical intervention, individuals can minimize the impact of hyperkeratosis on their skin health and overall well-being.
Visit Our Offices
Services:
- • Medical Dermatology
- • Surgical Dermatology
- • Laser Treatments
- • Cosmetic Dermatology
Services:
- • Medical Dermatology
- • Surgical Dermatology
- • Laser Treatments
- • Cosmetic Dermatology
Visit Our Offices
Services:
- • Medical Dermatology
- • Surgical Dermatology
- • Laser Treatments
- • Cosmetic Dermatology
Services:
- • Medical Dermatology
- • Surgical Dermatology
- • Laser Treatments
- • Cosmetic Dermatology