Granuloma: Dermatology Explained
A granuloma is a localized nodular inflammatory lesion formed by a collection of activated macrophages (often epithelioid cells and multinucleated giant cells) and lymphocytes that develops as a chronic immune response to persistent infection, foreign material, or immune-mediated stimuli.
Introduction to Granulomas
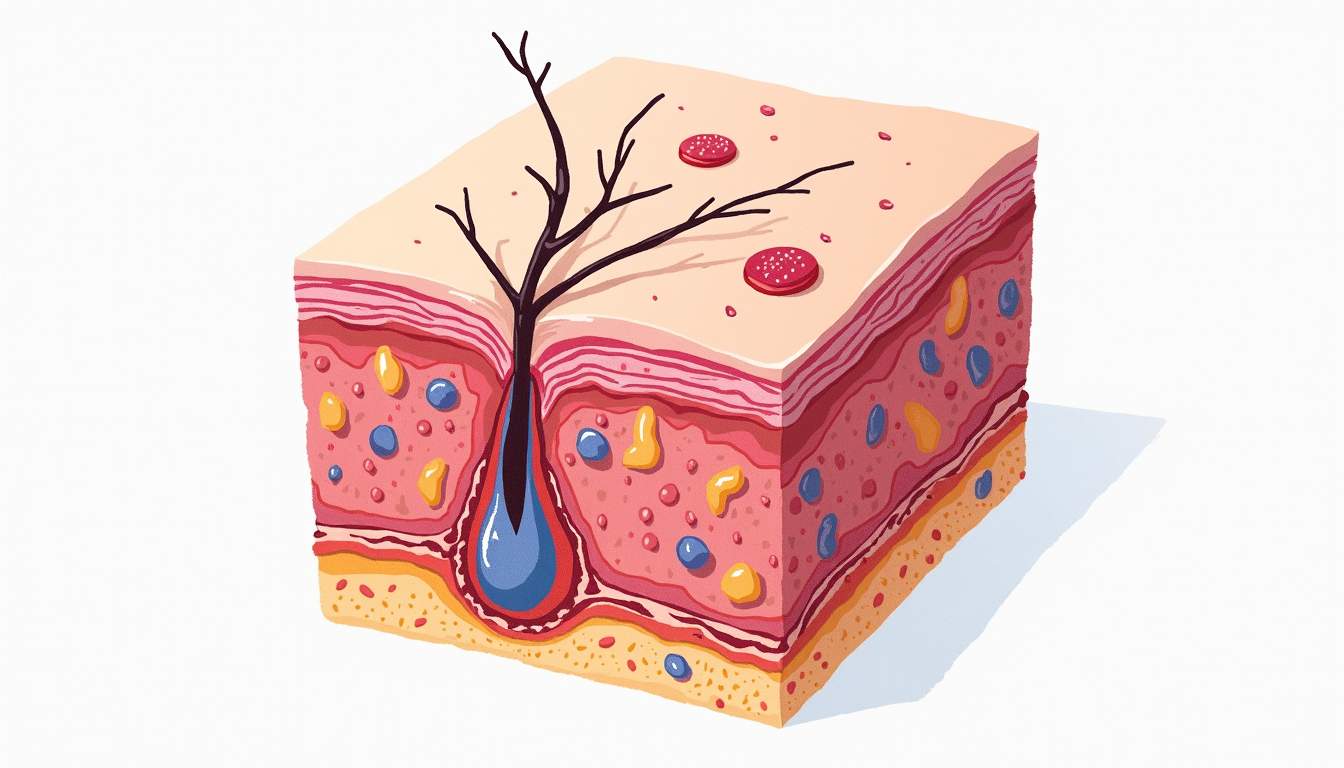
Granulomas are small areas of inflammation in tissue that occur as a response to infection, injury, or the presence of foreign substances. They are characterized by the aggregation of macrophages, which transform into epithelioid cells, and are often surrounded by lymphocytes and fibroblasts. This formation is a part of the body's immune response, aimed at isolating and containing the offending agents. Granulomas can occur in various organs, including the skin, lungs, and lymph nodes, and their presence can indicate a range of underlying conditions.
In dermatology, granulomas are particularly significant as they can manifest in various forms on the skin, often leading to diagnostic challenges. The appearance of granulomas can vary widely, and their identification is crucial for determining the appropriate treatment and management strategies. Understanding the pathophysiology, types, and clinical implications of granulomas is essential for dermatologists and healthcare providers.
This glossary entry will delve into the various aspects of granulomas, including their types, causes, clinical presentations, diagnostic methods, and treatment options. By providing a comprehensive overview, this article aims to equip readers with a thorough understanding of granulomas within the context of dermatology.
Types of Granulomas
Granulomas can be classified into several types based on their etiology, histological features, and clinical presentation. The most common types include:
- Non-caseating granulomas: These granulomas do not exhibit necrosis and are typically associated with conditions such as sarcoidosis and certain infections.
- Caseating granulomas: Characterized by central necrosis, these granulomas are often linked to infections like tuberculosis and certain fungal infections.
- Foreign body granulomas: These occur in response to the presence of foreign materials, such as sutures, talc, or silicone, and are characterized by the presence of multinucleated giant cells.
- Granuloma annulare: A benign condition that presents as ring-shaped lesions on the skin, often without any underlying systemic disease.
Each type of granuloma has distinct features that can aid in diagnosis. For instance, non-caseating granulomas are often seen in sarcoidosis, which can affect multiple organ systems, while caseating granulomas are typically indicative of infectious processes. Understanding these distinctions is crucial for dermatologists when evaluating patients presenting with granulomatous lesions.
Furthermore, granulomas can also be categorized based on their location, such as cutaneous granulomas, which specifically refer to granulomas that occur on the skin. This classification helps in understanding the clinical implications and potential systemic associations of the granulomatous response.
Causes of Granulomas
The formation of granulomas is a complex process that can be triggered by various factors. The most common causes include:
- Infections: Bacterial, viral, and fungal infections can lead to granuloma formation. For example, Mycobacterium tuberculosis is well-known for causing caseating granulomas in the lungs.
- Autoimmune diseases: Conditions such as sarcoidosis and Crohn's disease can result in the development of non-caseating granulomas as part of the immune response.
- Foreign bodies: The introduction of foreign materials into the skin or body can elicit a granulomatous response as the immune system attempts to isolate and eliminate the foreign substance.
- Drug reactions: Certain medications can cause granulomatous dermatitis, leading to the formation of granulomas on the skin.
In addition to these common causes, granulomas can also arise from chronic inflammatory conditions, such as eczema or psoriasis, where prolonged inflammation may lead to granuloma formation as a secondary response. The precise mechanism behind granuloma formation involves the activation of macrophages and the subsequent recruitment of other immune cells, which work together to contain and eliminate the offending agent.
Understanding the underlying causes of granulomas is essential for dermatologists, as it guides the diagnostic process and informs treatment decisions. A thorough patient history, including any recent infections, exposure to foreign materials, or medication use, can provide valuable insights into the etiology of the granulomatous lesions.
Clinical Presentation of Granulomas
Granulomas can present in various ways, depending on their type, location, and underlying cause. In dermatology, the clinical presentation can range from asymptomatic lesions to painful or pruritic nodules. Common features include:
- Appearance: Granulomas may appear as small, raised bumps (papules) or larger nodules on the skin. They can vary in color from skin-toned to red or brown, and may sometimes ulcerate or crust over.
- Distribution: The distribution of granulomas can be localized or widespread. For instance, granuloma annulare typically presents as ring-shaped lesions on the extremities, while foreign body granulomas may appear at the site of the foreign material.
- Symptoms: While many granulomas are asymptomatic, some may cause discomfort, itching, or tenderness, particularly if they are inflamed or infected.
In cases where granulomas are associated with systemic diseases, additional symptoms may be present, such as fever, weight loss, or respiratory symptoms, depending on the underlying condition. For example, patients with sarcoidosis may experience respiratory symptoms alongside cutaneous manifestations, necessitating a comprehensive evaluation.
Dermatologists must carefully assess the clinical presentation of granulomas, as this information is crucial for forming a differential diagnosis and determining the appropriate management plan. A thorough physical examination, along with a detailed patient history, can aid in identifying the specific type of granuloma and its potential associations.
Diagnostic Methods for Granulomas
Diagnosing granulomas involves a combination of clinical evaluation, laboratory tests, and histopathological examination. The following methods are commonly employed:
- Clinical examination: A thorough physical examination is the first step in diagnosing granulomas. Dermatologists assess the appearance, distribution, and symptoms of the lesions, which can provide valuable clues regarding the underlying cause.
- Laboratory tests: Blood tests may be conducted to evaluate for underlying systemic conditions, such as autoimmune diseases or infections. Specific tests, such as serum angiotensin-converting enzyme (ACE) levels, may be useful in diagnosing sarcoidosis.
- Skin biopsy: A definitive diagnosis often requires a skin biopsy, where a small sample of the affected tissue is removed and examined microscopically. Histopathological analysis can reveal the characteristic features of granulomas, including the presence of epithelioid cells and multinucleated giant cells.
In some cases, additional imaging studies, such as chest X-rays or CT scans, may be necessary to evaluate for systemic involvement, particularly in conditions like sarcoidosis or tuberculosis. The combination of clinical, laboratory, and histopathological findings allows dermatologists to arrive at an accurate diagnosis and formulate an appropriate treatment plan.
It is essential for dermatologists to remain vigilant in their diagnostic approach, as granulomas can mimic other skin conditions, such as infections, tumors, or inflammatory dermatoses. A comprehensive evaluation ensures that the correct diagnosis is made, leading to timely and effective management.
Treatment Options for Granulomas
The treatment of granulomas depends on the underlying cause, the type of granuloma, and the severity of the symptoms. Options may include:
- Observation: In cases where granulomas are asymptomatic and not associated with systemic disease, a watchful waiting approach may be appropriate, as many granulomas resolve spontaneously over time.
- Topical treatments: For localized granulomas, topical corticosteroids or calcineurin inhibitors may be effective in reducing inflammation and promoting healing.
- Intralesional injections: Corticosteroid injections directly into the granuloma can help reduce inflammation and size, particularly in cases of keloidal or hypertrophic granulomas.
- Systemic therapies: In cases where granulomas are associated with systemic diseases, such as sarcoidosis, systemic corticosteroids or immunosuppressive agents may be necessary to control the underlying condition.
In addition to these treatment options, addressing any underlying infections or foreign bodies is crucial for successful management. For instance, if a granuloma is caused by an infection, appropriate antimicrobial therapy should be initiated. Similarly, if a foreign body is identified, its removal may lead to resolution of the granulomatous response.
Dermatologists must tailor treatment plans to the individual patient, taking into consideration the type of granuloma, the patient's overall health, and any potential side effects of the chosen therapies. A multidisciplinary approach may be beneficial in complex cases, involving collaboration with other specialists, such as infectious disease experts or rheumatologists, to ensure comprehensive care.
Prognosis and Follow-Up
The prognosis for patients with granulomas varies widely depending on the underlying cause and the type of granuloma. Many granulomas, particularly those that are benign and localized, may resolve spontaneously without treatment. However, granulomas associated with systemic diseases may require ongoing management and monitoring.
Follow-up care is essential for patients with granulomas, especially those with underlying conditions that may necessitate long-term treatment. Regular monitoring can help assess the response to therapy, identify any potential complications, and ensure that the granulomatous lesions are not indicative of a more serious underlying condition.
In cases where granulomas are persistent or recurrent, further evaluation may be warranted to rule out other underlying issues. Dermatologists should maintain open communication with patients regarding their condition, treatment options, and any changes in symptoms, fostering a collaborative approach to care.
Conclusion
Granulomas represent a fascinating and complex aspect of dermatology, reflecting the body's immune response to various stimuli. Understanding the types, causes, clinical presentations, diagnostic methods, and treatment options for granulomas is essential for dermatologists and healthcare providers. By recognizing the significance of granulomas and their potential implications, clinicians can provide effective care and improve patient outcomes.
As research continues to evolve in the field of dermatology, further insights into the mechanisms of granuloma formation and resolution may lead to more targeted therapies and improved management strategies. For patients, understanding their condition and the rationale behind treatment options can empower them to take an active role in their healthcare journey.
In summary, granulomas are a key topic within dermatology that warrants careful consideration and comprehensive management. By staying informed and engaged, both clinicians and patients can navigate the complexities of granulomas and work towards achieving optimal health outcomes.
Visit Our Offices
Services:
- • Medical Dermatology
- • Surgical Dermatology
- • Laser Treatments
- • Cosmetic Dermatology
Services:
- • Medical Dermatology
- • Surgical Dermatology
- • Laser Treatments
- • Cosmetic Dermatology
Visit Our Offices
Services:
- • Medical Dermatology
- • Surgical Dermatology
- • Laser Treatments
- • Cosmetic Dermatology
Services:
- • Medical Dermatology
- • Surgical Dermatology
- • Laser Treatments
- • Cosmetic Dermatology