Introduction to Follicular Occlusion
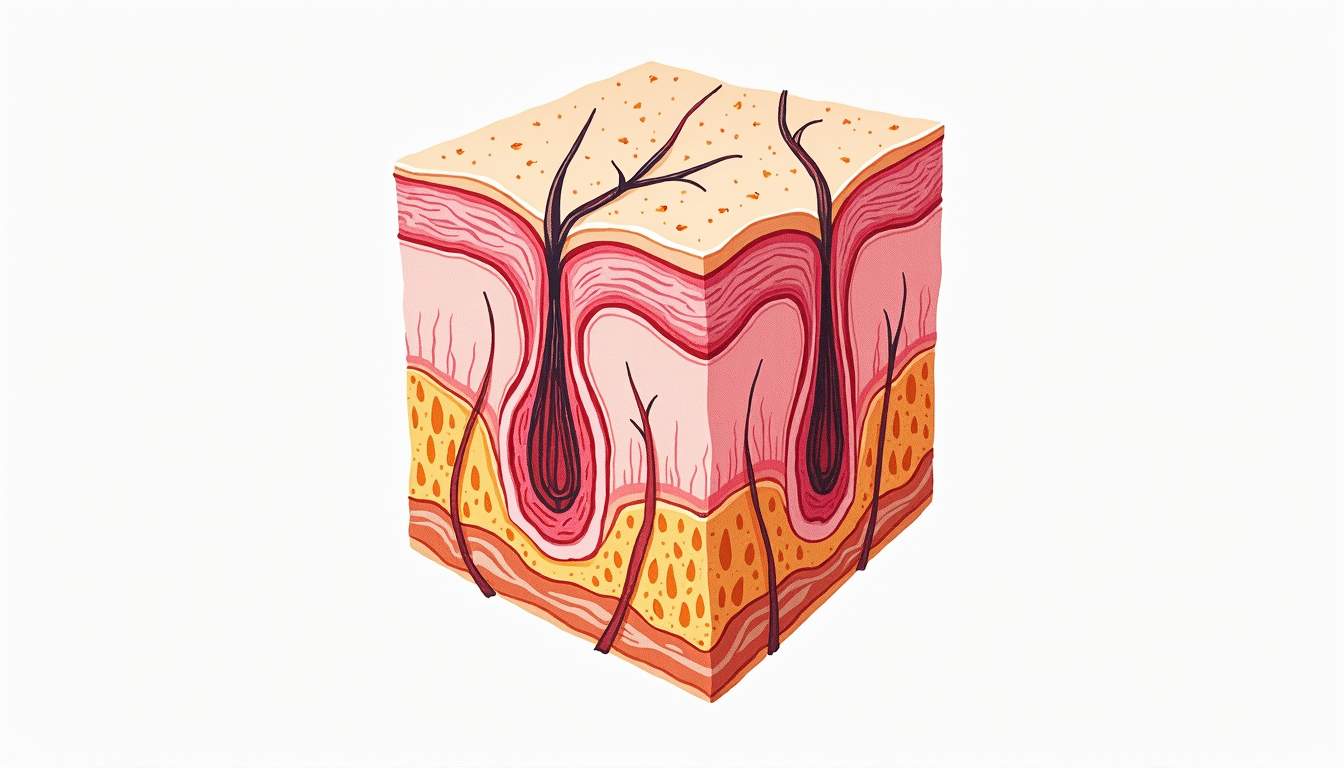
Follicular occlusion is a term used in dermatology to describe a condition where hair follicles become blocked or obstructed. This blockage can lead to various skin issues, including inflammation, infection, and the formation of lesions. Understanding follicular occlusion is crucial for dermatologists and healthcare providers, as it plays a significant role in several dermatological disorders, including acne, hidradenitis suppurativa, and folliculitis. The pathophysiology of follicular occlusion involves a complex interplay of factors, including genetics, environmental influences, and immune responses.
Follicular occlusion can manifest in different ways, depending on the underlying cause and the individual's skin type. It is essential to recognize the signs and symptoms associated with this condition to provide appropriate treatment and management. In this glossary entry, we will explore the various aspects of follicular occlusion, including its causes, symptoms, diagnosis, treatment options, and its relationship with other dermatological conditions.
Causes of Follicular Occlusion
The causes of follicular occlusion can be multifactorial. Understanding these causes is vital for effective treatment and management. Here are some of the primary factors contributing to follicular occlusion:
1. Genetics
Genetic predisposition plays a significant role in the development of follicular occlusion. Certain individuals may inherit traits that make them more susceptible to conditions that cause follicular blockage. For example, genetic mutations affecting keratinization can lead to abnormal skin cell turnover, resulting in the accumulation of dead skin cells within the hair follicle. This accumulation can ultimately lead to occlusion and inflammation.
2. Hormonal Influences
Hormonal changes, particularly those related to androgens, can significantly impact the health of hair follicles. Androgens can stimulate sebaceous glands, leading to increased oil production. When excess sebum combines with dead skin cells, it can clog hair follicles, resulting in follicular occlusion. This is particularly evident in conditions such as acne, where hormonal fluctuations during puberty, menstruation, or pregnancy can exacerbate the blockage.
3. Environmental Factors
Environmental factors, including exposure to pollutants, humidity, and friction, can also contribute to follicular occlusion. For instance, wearing tight clothing or using heavy cosmetics can create an environment conducive to follicular blockage. Additionally, exposure to certain chemicals or irritants can disrupt the normal functioning of hair follicles, leading to inflammation and occlusion.
4. Skin Conditions
Various skin conditions can lead to follicular occlusion. Conditions such as acne vulgaris, folliculitis, and hidradenitis suppurativa are characterized by inflammation and blockage of hair follicles. In these cases, the underlying pathophysiology involves a combination of factors, including bacterial overgrowth, immune dysregulation, and abnormal keratinization. Understanding these conditions is essential for effective management and treatment.
Symptoms of Follicular Occlusion
The symptoms of follicular occlusion can vary depending on the severity of the condition and the specific underlying cause. Common symptoms include:
1. Inflammation
Inflammation is a hallmark symptom of follicular occlusion. Affected areas may appear red, swollen, and tender to the touch. This inflammatory response is often a result of the body's immune system reacting to the blockage within the hair follicle. In some cases, the inflammation can lead to the formation of pustules or nodules, which may be painful and uncomfortable.
2. Lesions
Follicular occlusion can lead to the development of various types of skin lesions. These may include comedones (blackheads and whiteheads), papules, pustules, and cysts. The type of lesion formed often depends on the extent of the blockage and the presence of secondary infections. For instance, in acne vulgaris, comedones are commonly observed, while hidradenitis suppurativa may present with painful nodules and abscesses.
3. Itching and Discomfort
Individuals experiencing follicular occlusion may also report itching and discomfort in the affected areas. This sensation can be attributed to the inflammatory response and the irritation caused by the blockage. Scratching or picking at the lesions can exacerbate the condition and lead to further complications, such as secondary infections or scarring.
Diagnosis of Follicular Occlusion
Diagnosing follicular occlusion involves a comprehensive evaluation of the patient's medical history, clinical examination, and, in some cases, laboratory tests. Dermatologists typically follow a systematic approach to arrive at an accurate diagnosis.
1. Medical History
A thorough medical history is essential in understanding the patient's symptoms and potential triggers for follicular occlusion. Dermatologists will inquire about the duration and severity of symptoms, any previous treatments, family history of skin conditions, and lifestyle factors that may contribute to the condition. This information helps in identifying patterns and potential underlying causes.
2. Clinical Examination
A clinical examination involves a visual assessment of the skin and affected areas. Dermatologists will look for characteristic signs of follicular occlusion, such as the presence of comedones, papules, pustules, or cysts. They may also assess the distribution of lesions, as certain conditions may present in specific areas of the body. In some cases, a dermatoscopic examination may be performed to gain a closer look at the hair follicles and surrounding skin.
3. Laboratory Tests
In certain situations, laboratory tests may be necessary to confirm the diagnosis or rule out other conditions. For example, a skin biopsy may be performed to examine the histopathology of the lesions. Additionally, cultures may be taken to identify any bacterial or fungal infections that could be contributing to the follicular occlusion. Blood tests may also be ordered to evaluate hormonal levels if hormonal influences are suspected.
Treatment Options for Follicular Occlusion
Treatment for follicular occlusion aims to address the underlying causes, alleviate symptoms, and prevent complications. The choice of treatment depends on the severity of the condition and the specific diagnosis. Common treatment options include:
1. Topical Treatments
Topical treatments are often the first line of defense against follicular occlusion. These may include:
- Retinoids: Topical retinoids, such as tretinoin and adapalene, help normalize skin cell turnover and prevent the formation of comedones.
- Antibiotics: Topical antibiotics, such as clindamycin or erythromycin, can reduce bacterial overgrowth and inflammation associated with follicular occlusion.
- Salicylic Acid: This beta-hydroxy acid helps exfoliate the skin and unclog pores, making it effective for treating acne and folliculitis.
2. Oral Medications
In more severe cases, oral medications may be necessary to manage follicular occlusion. These may include:
- Oral Antibiotics: Medications such as doxycycline or minocycline can help reduce inflammation and bacterial load in cases of severe acne or hidradenitis suppurativa.
- Hormonal Treatments: For individuals with hormonal influences contributing to follicular occlusion, hormonal therapies such as oral contraceptives or anti-androgens may be prescribed.
- Isotretinoin: In cases of severe, treatment-resistant acne, isotretinoin may be considered. This powerful medication reduces sebum production and prevents the formation of new lesions.
3. Surgical Interventions
In certain situations, surgical interventions may be necessary to address follicular occlusion. These may include:
- Incision and Drainage: For painful cysts or abscesses, a healthcare provider may perform an incision and drainage procedure to relieve pressure and remove the contents.
- Laser Therapy: Laser treatments can be effective in reducing inflammation and scarring associated with follicular occlusion, particularly in cases of hidradenitis suppurativa.
- Excision: In chronic cases of hidradenitis suppurativa, surgical excision of affected areas may be necessary to prevent recurrence and improve quality of life.
Relationship with Other Dermatological Conditions
Follicular occlusion is not an isolated condition; rather, it is often associated with several other dermatological disorders. Understanding these relationships is essential for comprehensive patient care.
1. Acne Vulgaris
Acne vulgaris is one of the most common conditions associated with follicular occlusion. The blockage of hair follicles due to excess sebum and dead skin cells leads to the formation of comedones, papules, and pustules. Hormonal fluctuations, particularly during puberty, can exacerbate this condition, making it a prime example of how follicular occlusion manifests in everyday dermatological practice.
2. Hidradenitis Suppurativa
Hidradenitis suppurativa is a chronic inflammatory skin condition characterized by recurrent abscesses and scarring. It is closely linked to follicular occlusion, as the condition primarily affects areas with a high density of hair follicles, such as the armpits and groin. The pathophysiology of hidradenitis suppurativa involves a combination of follicular occlusion, immune dysregulation, and bacterial overgrowth.
3. Folliculitis
Folliculitis is an inflammation of the hair follicles that can occur due to bacterial, fungal, or viral infections. While it may not always be directly caused by follicular occlusion, the two conditions can coexist. Follicular occlusion can create an environment conducive to infection, leading to folliculitis. Treatment for folliculitis often involves addressing the underlying occlusion to prevent recurrence.
Conclusion
Follicular occlusion is a complex dermatological condition that can significantly impact an individual's skin health and quality of life. Understanding its causes, symptoms, diagnosis, and treatment options is essential for effective management. By recognizing the relationship between follicular occlusion and other dermatological disorders, healthcare providers can offer comprehensive care tailored to each patient's needs. Ongoing research and advancements in dermatology continue to shed light on the intricacies of follicular occlusion, paving the way for improved treatment strategies and patient outcomes.
Visit Our Offices
Services:
- • Medical Dermatology
- • Surgical Dermatology
- • Laser Treatments
- • Cosmetic Dermatology
Services:
- • Medical Dermatology
- • Surgical Dermatology
- • Laser Treatments
- • Cosmetic Dermatology
Visit Our Offices
Services:
- • Medical Dermatology
- • Surgical Dermatology
- • Laser Treatments
- • Cosmetic Dermatology
Services:
- • Medical Dermatology
- • Surgical Dermatology
- • Laser Treatments
- • Cosmetic Dermatology