Introduction to Comedones
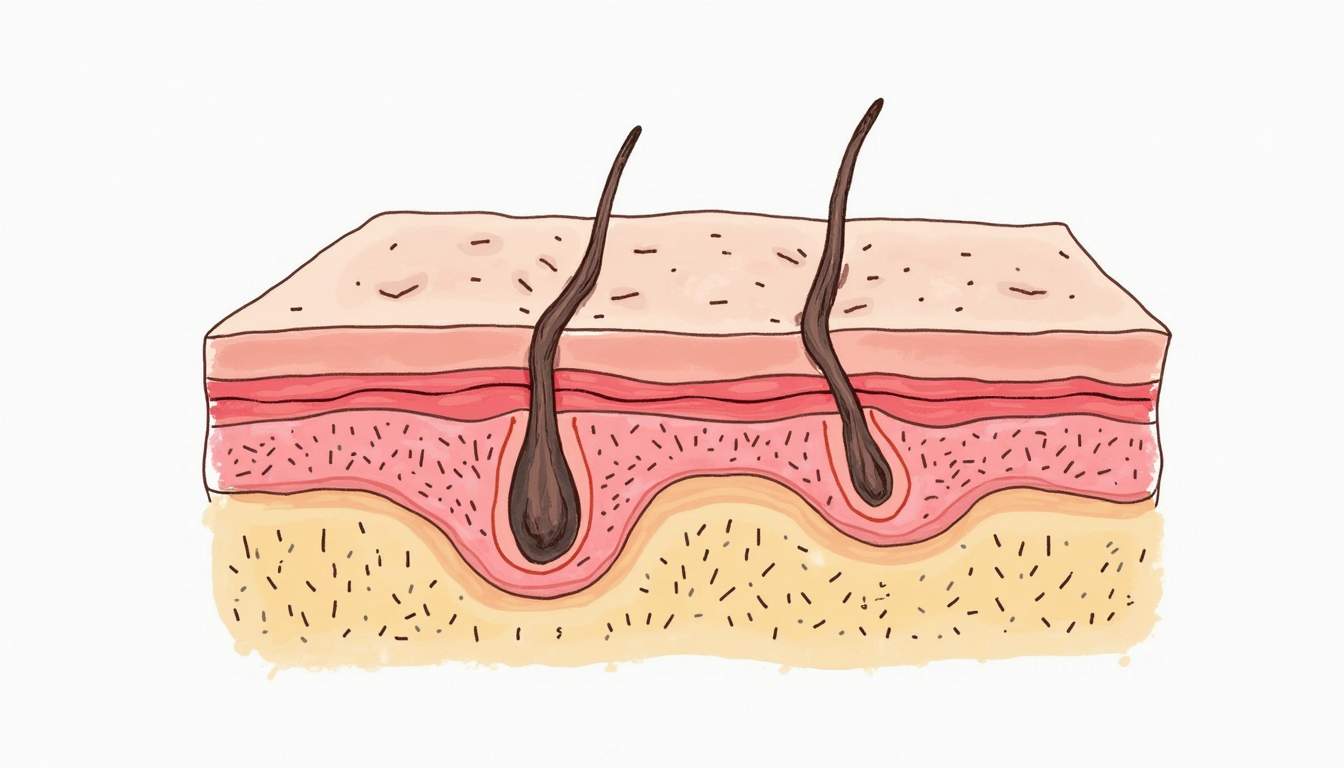
Comedones are a type of acne lesion that forms when hair follicles become clogged with oil, dead skin cells, and bacteria. They are one of the most common skin conditions encountered in dermatology and can appear on various parts of the body, including the face, neck, back, and shoulders. Understanding the nature of comedones is crucial for effective treatment and prevention strategies.
There are two primary types of comedones: open comedones, commonly known as blackheads, and closed comedones, referred to as whiteheads. The distinction between these two types is based on whether the follicle is open or closed at the skin's surface. This glossary entry will delve into the characteristics, causes, and treatment options for both types of comedones.
In dermatology, the management of comedones is essential not only for cosmetic reasons but also for preventing the progression of acne. Untreated comedones can lead to more severe forms of acne, including papules, pustules, and cysts. Therefore, a comprehensive understanding of comedones is vital for both patients and healthcare providers.
Types of Comedones
Open Comedones (Blackheads)
Open comedones, or blackheads, are characterized by their dark appearance, which is due to the oxidation of melanin in the clogged follicle. The follicle remains open at the skin's surface, allowing air to come into contact with the trapped material. This exposure leads to the characteristic dark color, which is often mistaken for dirt or debris.
Blackheads are commonly found on the nose, forehead, and chin, areas known as the T-zone. They can be more prevalent in individuals with oily skin, as excess sebum production contributes to the clogging of pores. Although blackheads are not inflammatory, they can be a source of frustration for many individuals seeking clear skin.
Management of open comedones often involves topical treatments that promote exfoliation and reduce oiliness. Ingredients such as salicylic acid, benzoyl peroxide, and retinoids are commonly used to help unclog pores and prevent the formation of new blackheads.
Closed Comedones (Whiteheads)
Closed comedones, or whiteheads, occur when the follicle is completely blocked, preventing air from entering. This results in a small, flesh-colored or white bump on the skin's surface. Unlike blackheads, whiteheads do not have the same dark pigmentation due to the absence of oxidation.
Whiteheads can be more challenging to treat than blackheads, as they are often deeper within the skin. They are frequently associated with hormonal changes, such as those experienced during puberty or menstruation, and can also be exacerbated by the use of heavy cosmetics or skincare products that clog pores.
Effective treatment for closed comedones may include the use of topical retinoids, which help to promote cell turnover and prevent the formation of new comedones. In some cases, dermatologists may recommend extraction procedures to remove stubborn whiteheads.
Causes of Comedones
Excess Sebum Production
One of the primary causes of comedones is excess sebum production by the sebaceous glands. Sebum is an oily substance that helps to keep the skin moisturized. However, when produced in excess, it can lead to clogged pores, resulting in the formation of comedones. Factors that can contribute to increased sebum production include hormonal fluctuations, particularly androgens, which stimulate the sebaceous glands.
Hormonal changes during puberty, menstruation, pregnancy, and the use of hormonal contraceptives can all influence sebum production. Additionally, certain medications, such as corticosteroids, can also lead to increased oiliness of the skin, further contributing to the development of comedones.
Dead Skin Cells
Another significant factor in the formation of comedones is the accumulation of dead skin cells. The skin naturally sheds dead cells, but when this process is disrupted, these cells can build up within hair follicles. This blockage can trap sebum and bacteria, leading to the development of both open and closed comedones.
Improper exfoliation practices, whether due to the use of harsh scrubs or inadequate skincare routines, can exacerbate the issue. Regular exfoliation, whether through physical or chemical means, is essential for maintaining clear pores and preventing the formation of comedones.
Bacterial Growth
The presence of bacteria, particularly Propionibacterium acnes, plays a role in the development of comedones. While comedones themselves are not inflammatory, the presence of bacteria can lead to inflammation and the progression of acne. When hair follicles become clogged, bacteria can thrive in the anaerobic environment, potentially leading to the formation of papules and pustules.
Maintaining a balanced skin microbiome and using antibacterial agents can help reduce the risk of bacterial overgrowth and subsequent acne development. Incorporating products with antibacterial properties, such as benzoyl peroxide, can be beneficial in managing comedones and preventing further complications.
Diagnosis of Comedones
The diagnosis of comedones is typically made through a physical examination by a dermatologist. The clinician will assess the skin's appearance, noting the presence of blackheads and whiteheads, as well as any associated inflammation. In most cases, no additional testing is required, as the visual identification of comedones is usually sufficient for diagnosis.
In some instances, a dermatologist may inquire about the patient's medical history, including any previous skin conditions, family history of acne, and current skincare routines. This information can help guide treatment recommendations and identify potential contributing factors to the patient's comedonal acne.
For patients with persistent or severe cases of comedones, further evaluation may be warranted to rule out underlying hormonal imbalances or other dermatological conditions. In such cases, blood tests or hormonal assessments may be conducted to provide a comprehensive understanding of the patient's skin health.
Treatment Options for Comedones
Topical Treatments
Topical treatments are often the first line of defense in managing comedones. These treatments aim to unclog pores, reduce oiliness, and promote cell turnover. Commonly used topical agents include:
- Salicylic Acid: A beta-hydroxy acid that penetrates the pores to dissolve excess oil and dead skin cells.
- Benzoyl Peroxide: An antibacterial agent that helps reduce inflammation and prevent the growth of acne-causing bacteria.
- Retinoids: Vitamin A derivatives that promote cell turnover, helping to prevent the formation of new comedones.
- Alpha Hydroxy Acids (AHAs): Water-soluble acids that exfoliate the surface of the skin, improving texture and reducing the appearance of comedones.
These topical treatments can be used individually or in combination, depending on the severity of the comedonal acne and the patient's skin type. It is important for patients to follow their dermatologist's recommendations regarding the frequency and method of application to achieve optimal results.
Professional Treatments
For individuals with persistent comedones that do not respond to topical treatments, professional interventions may be necessary. Dermatologists can perform various procedures to effectively manage comedones, including:
- Comedone Extraction: A procedure in which a dermatologist uses specialized tools to manually extract blackheads and whiteheads from the skin.
- Chemical Peels: Treatments that involve the application of chemical exfoliants to the skin, promoting the shedding of dead skin cells and unclogging pores.
- Microdermabrasion: A non-invasive procedure that exfoliates the outer layer of skin, helping to improve texture and reduce the appearance of comedones.
- Laser Therapy: Certain laser treatments can target oil glands and reduce sebum production, helping to prevent the formation of comedones.
These professional treatments can provide more immediate results and may be particularly beneficial for individuals with severe or stubborn comedonal acne. Patients should consult with their dermatologist to determine the most appropriate treatment plan based on their specific needs and skin type.
Prevention of Comedones
Preventing the formation of comedones involves adopting a consistent skincare routine and making lifestyle choices that promote healthy skin. Some effective prevention strategies include:
- Regular Cleansing: Cleansing the skin twice daily with a gentle, non-comedogenic cleanser can help remove excess oil and prevent clogged pores.
- Exfoliation: Incorporating regular exfoliation into the skincare routine can help remove dead skin cells and prevent buildup in hair follicles.
- Non-Comedogenic Products: Choosing skincare and makeup products labeled as non-comedogenic can help reduce the risk of pore clogging.
- Healthy Diet: A balanced diet rich in fruits, vegetables, and whole grains can support overall skin health and may help reduce acne flare-ups.
Additionally, individuals should avoid picking or squeezing comedones, as this can lead to inflammation, scarring, and further acne development. Maintaining a consistent skincare routine and being mindful of product ingredients can significantly reduce the likelihood of developing comedones.
Conclusion
Comedones are a common skin condition that can affect individuals of all ages. Understanding the different types of comedones, their causes, and effective treatment options is essential for managing this condition and preventing its progression to more severe forms of acne. By adopting a comprehensive approach that includes proper skincare, professional treatments, and lifestyle modifications, individuals can achieve clearer skin and improve their overall skin health.
As with any dermatological concern, it is important for individuals to consult with a qualified dermatologist for personalized recommendations and treatment plans tailored to their specific needs. With the right knowledge and resources, managing comedones and achieving healthy skin is entirely possible.
Visit Our Offices
Services:
- • Medical Dermatology
- • Surgical Dermatology
- • Laser Treatments
- • Cosmetic Dermatology
Services:
- • Medical Dermatology
- • Surgical Dermatology
- • Laser Treatments
- • Cosmetic Dermatology
Visit Our Offices
Services:
- • Medical Dermatology
- • Surgical Dermatology
- • Laser Treatments
- • Cosmetic Dermatology
Services:
- • Medical Dermatology
- • Surgical Dermatology
- • Laser Treatments
- • Cosmetic Dermatology