Atopic Dermatitis: Dermatology Explained
A chronic, itchy inflammatory skin condition—often beginning in childhood—characterized by dry, eczematous lesions and driven by genetic, immune, and environmental factors, frequently associated with other allergic diseases.
Introduction to Atopic Dermatitis
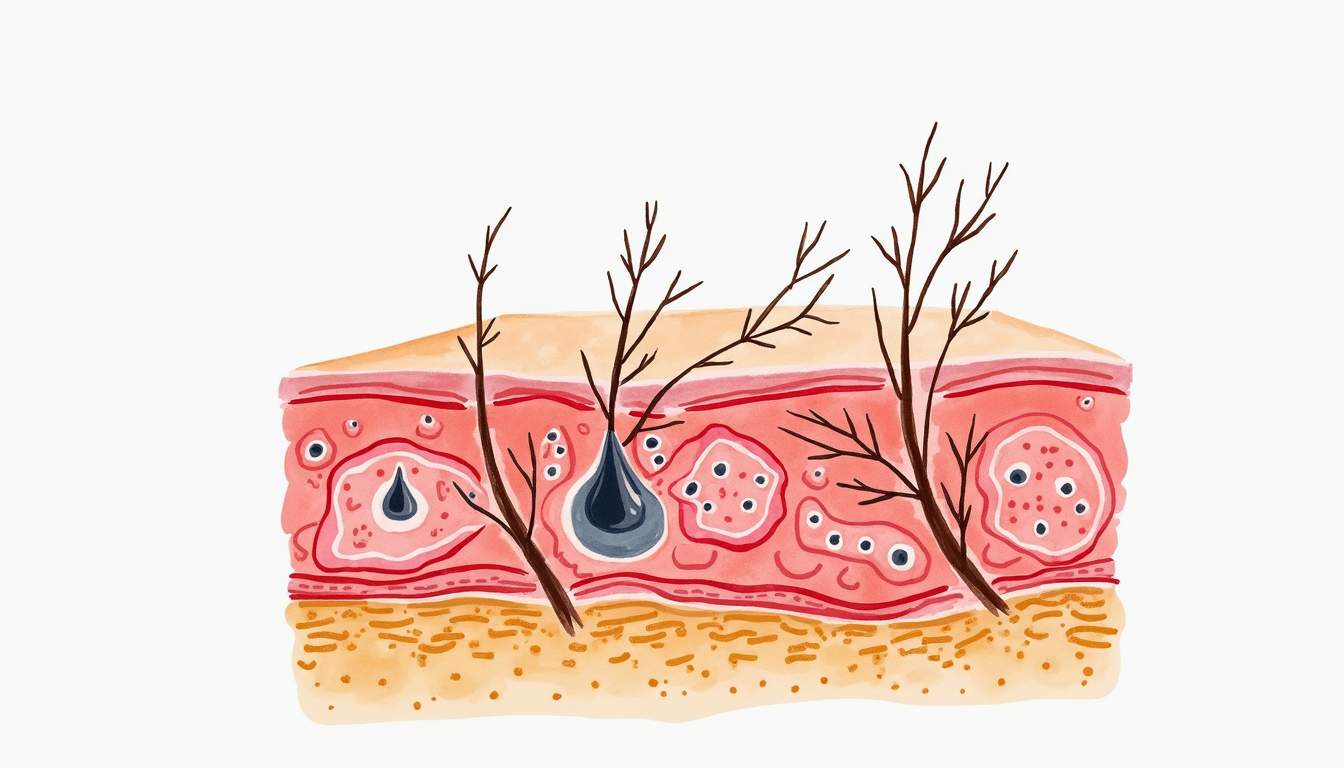
Atopic dermatitis (AD), commonly referred to as eczema, is a chronic inflammatory skin condition characterized by dry, itchy, and inflamed skin. It is a common condition, particularly among children, but it can persist into adulthood. The etiology of atopic dermatitis is multifactorial, involving genetic, environmental, and immunological factors. Understanding the pathophysiology of atopic dermatitis is essential for effective management and treatment.
Atopic dermatitis is part of a group of conditions known as atopic diseases, which also includes asthma and allergic rhinitis. These conditions often coexist, and individuals with atopic dermatitis are at an increased risk of developing other allergic conditions. The prevalence of atopic dermatitis has been rising globally, making it a significant public health concern.
In this glossary entry, we will explore the various aspects of atopic dermatitis, including its causes, symptoms, diagnosis, treatment options, and management strategies. We will also discuss the impact of atopic dermatitis on the quality of life and the importance of patient education in managing this chronic condition.
Causes of Atopic Dermatitis
Genetic Factors
Genetic predisposition plays a crucial role in the development of atopic dermatitis. Studies have shown that individuals with a family history of atopic diseases are more likely to develop AD. Mutations in the filaggrin gene (FLG) have been identified as a significant risk factor for atopic dermatitis. Filaggrin is a protein that helps maintain the skin barrier, and its deficiency can lead to increased transepidermal water loss and susceptibility to irritants and allergens.
Other genetic components may also contribute to the dysregulation of the immune system seen in atopic dermatitis. Variations in genes associated with immune response, such as those involved in the production of cytokines and chemokines, can influence the severity and course of the disease. Understanding these genetic factors is essential for developing targeted therapies and personalized treatment approaches.
Environmental Factors
Environmental factors play a significant role in the exacerbation of atopic dermatitis. Common triggers include exposure to allergens such as pollen, dust mites, pet dander, and certain foods. Irritants like soaps, detergents, and fragrances can also worsen symptoms. Additionally, environmental conditions such as low humidity, extreme temperatures, and pollution can contribute to skin barrier dysfunction and increased inflammation.
Stress is another environmental factor that can exacerbate atopic dermatitis. Psychological stress can lead to the release of pro-inflammatory cytokines, which may worsen skin inflammation. Identifying and managing environmental triggers is crucial for effective long-term management of atopic dermatitis.
Symptoms of Atopic Dermatitis
Common Symptoms
The symptoms of atopic dermatitis can vary widely among individuals and may change over time. The most common symptoms include intense itching, dry skin, and the presence of red, inflamed patches on the skin. These patches may appear on various parts of the body, including the face, neck, hands, and the insides of the elbows and knees.
In infants, atopic dermatitis often presents as crusty, oozing lesions, particularly on the scalp and face. As children grow, the distribution of the rash may change, and the skin may become thickened and leathery due to chronic scratching. Secondary infections can also occur due to skin barrier impairment, leading to further complications.
Chronic Symptoms and Flare-Ups
Atopic dermatitis is characterized by periods of flare-ups followed by remissions. During flare-ups, symptoms can become significantly worse, leading to increased discomfort and distress for the affected individual. Chronic scratching and rubbing can lead to lichenification, where the skin becomes thickened and darkened due to prolonged inflammation.
In addition to physical symptoms, atopic dermatitis can have psychological effects, including anxiety and depression, particularly in adolescents and adults. The visibility of skin lesions and the chronic nature of the condition can lead to social stigma and reduced quality of life.
Diagnosis of Atopic Dermatitis
Clinical Evaluation
The diagnosis of atopic dermatitis is primarily based on clinical evaluation and the patient's medical history. Dermatologists assess the characteristic appearance of the skin lesions, distribution of the rash, and associated symptoms such as itching. A thorough history of the patient's family and personal history of atopic diseases is also crucial in establishing a diagnosis.
In some cases, additional tests may be performed to rule out other skin conditions that may mimic atopic dermatitis, such as contact dermatitis or psoriasis. Patch testing may be conducted to identify specific allergens that could be contributing to the patient's symptoms.
Diagnostic Criteria
Several diagnostic criteria have been established to aid in the diagnosis of atopic dermatitis. The Hanifin and Rajka criteria are widely used and include major and minor criteria. Major criteria include pruritus, typical morphology and distribution of lesions, and a chronic or relapsing course. Minor criteria encompass a range of features, including a personal or family history of atopy, dry skin, and elevated serum IgE levels.
Accurate diagnosis is essential for effective management and treatment planning. Misdiagnosis can lead to inappropriate treatment and worsening of symptoms, highlighting the importance of a comprehensive evaluation by a qualified healthcare professional.
Treatment Options for Atopic Dermatitis
Topical Treatments
Topical treatments are the cornerstone of managing atopic dermatitis. Emollients and moisturizers are essential for maintaining skin hydration and restoring the skin barrier. These products should be applied regularly, even when the skin appears clear, to prevent flare-ups.
Topical corticosteroids are commonly prescribed to reduce inflammation and itching during flare-ups. The potency of the corticosteroid should be matched to the severity of the condition and the area of the body being treated. For sensitive areas, such as the face and groin, lower-potency corticosteroids are recommended to minimize the risk of side effects.
Systemic Treatments
In cases of moderate to severe atopic dermatitis that do not respond to topical treatments, systemic therapies may be considered. These include oral corticosteroids, immunosuppressants, and biologic therapies. Oral corticosteroids can provide rapid relief but are not recommended for long-term use due to potential side effects.
Immunosuppressants such as cyclosporine and methotrexate may be used for chronic cases, but they require careful monitoring due to their potential adverse effects on the immune system. Biologic therapies, such as dupilumab, have emerged as a promising option for patients with moderate to severe atopic dermatitis, targeting specific pathways in the immune response.
Management Strategies for Atopic Dermatitis
Patient Education
Patient education is a vital component of managing atopic dermatitis. Patients and caregivers should be informed about the nature of the condition, potential triggers, and the importance of adherence to treatment regimens. Understanding the chronic nature of atopic dermatitis can help patients set realistic expectations and reduce frustration associated with flare-ups.
Education should also include guidance on proper skincare routines, including the use of emollients and moisturizers, as well as techniques for managing itching and preventing secondary infections. Support groups and educational resources can provide additional support for patients and families coping with the challenges of atopic dermatitis.
Lifestyle Modifications
Lifestyle modifications can play a significant role in managing atopic dermatitis. Patients should be encouraged to identify and avoid known triggers, such as specific allergens or irritants. Maintaining a consistent skincare routine that includes regular moisturizing can help improve skin barrier function and reduce the frequency of flare-ups.
Stress management techniques, such as mindfulness, yoga, or counseling, may also be beneficial in reducing the psychological impact of atopic dermatitis. A holistic approach that addresses both physical and emotional well-being is essential for effective management of this chronic condition.
Impact on Quality of Life
Physical and Emotional Effects
Atopic dermatitis can significantly impact an individual's quality of life. The physical symptoms, including itching and discomfort, can interfere with daily activities, sleep, and overall well-being. Chronic scratching can lead to skin damage and secondary infections, further complicating the condition.
Emotionally, individuals with atopic dermatitis may experience feelings of embarrassment, frustration, and social isolation due to the visible nature of the skin lesions. Children with atopic dermatitis may face bullying or teasing, leading to low self-esteem and anxiety. Addressing these emotional aspects is crucial for comprehensive care and support.
Social and Economic Implications
The social implications of atopic dermatitis extend beyond the individual, affecting family dynamics and relationships. Caregivers may experience stress and fatigue due to the demands of managing a chronic condition. Additionally, the economic burden of atopic dermatitis can be substantial, with costs associated with medical treatments, over-the-counter products, and lost productivity due to missed work or school days.
Raising awareness about atopic dermatitis and its impact on quality of life is essential for fostering understanding and support within communities. Advocacy efforts can help improve access to care and resources for individuals affected by this condition.
Conclusion
Atopic dermatitis is a complex and multifaceted condition that requires a comprehensive approach to management. Understanding the underlying causes, recognizing symptoms, and implementing effective treatment strategies are essential for improving patient outcomes. Ongoing research into the pathophysiology of atopic dermatitis and the development of new therapies holds promise for better management of this chronic skin condition.
Through patient education, lifestyle modifications, and a supportive healthcare environment, individuals with atopic dermatitis can lead fulfilling lives despite the challenges posed by this condition. Collaborative efforts among healthcare providers, patients, and families are crucial for achieving optimal management and improving the quality of life for those affected by atopic dermatitis.
Visit Our Offices
Services:
- • Medical Dermatology
- • Surgical Dermatology
- • Laser Treatments
- • Cosmetic Dermatology
Services:
- • Medical Dermatology
- • Surgical Dermatology
- • Laser Treatments
- • Cosmetic Dermatology
Visit Our Offices
Services:
- • Medical Dermatology
- • Surgical Dermatology
- • Laser Treatments
- • Cosmetic Dermatology
Services:
- • Medical Dermatology
- • Surgical Dermatology
- • Laser Treatments
- • Cosmetic Dermatology