Acne Vulgaris: Dermatology Explained
A common inflammatory disorder of the pilosebaceous units characterized by comedones, papules, pustules, and sometimes nodules caused by increased sebum production, follicular hyperkeratinization, Cutibacterium acnes proliferation, and inflammation.
Introduction to Acne Vulgaris
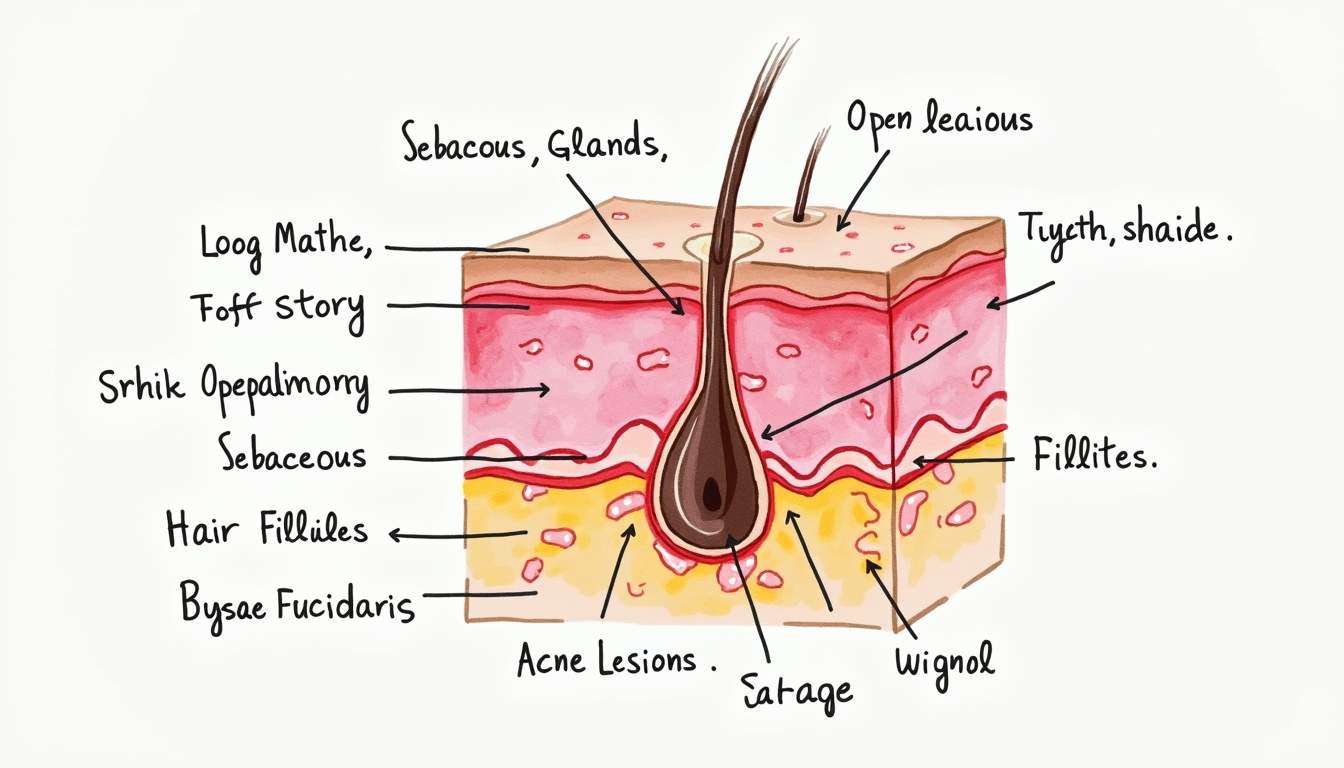
Acne vulgaris, commonly referred to simply as acne, is a multifactorial skin condition that primarily affects the pilosebaceous units of the skin. It is characterized by the presence of comedones (clogged hair follicles), papules, pustules, and, in more severe cases, nodules and cysts. Acne vulgaris is most prevalent during adolescence but can occur at any age, affecting both males and females. The condition can have significant psychological impacts, including low self-esteem and depression, making its understanding and treatment essential in dermatology.
Acne vulgaris is not merely a cosmetic issue; it is a chronic inflammatory disease that can lead to scarring and hyperpigmentation if not managed properly. The pathophysiology of acne involves a complex interplay of hormonal changes, increased sebum production, follicular hyperkeratinization, and the proliferation of Cutibacterium acnes, a bacterium that is part of the normal skin flora. Understanding these mechanisms is crucial for effective treatment and management strategies.
Pathophysiology of Acne Vulgaris
Hormonal Influences
One of the primary factors contributing to the development of acne vulgaris is hormonal changes, particularly during puberty. Androgens, such as testosterone, stimulate the sebaceous glands to produce more sebum, which can lead to clogged pores. This increase in sebum production is often exacerbated by hormonal fluctuations associated with menstrual cycles, pregnancy, and certain endocrine disorders. Understanding the hormonal influences on acne is vital for developing targeted treatments, especially in female patients.
In addition to androgens, other hormones, such as insulin and insulin-like growth factor 1 (IGF-1), have been implicated in acne pathogenesis. Elevated levels of these hormones can increase sebum production and promote follicular hyperkeratinization, further contributing to the development of acne lesions. This hormonal interplay underscores the importance of a comprehensive approach to acne treatment that may include hormonal therapies in certain cases.
Microbial Factors
Cutibacterium acnes, previously known as Propionibacterium acnes, is a gram-positive anaerobic bacterium that plays a significant role in the pathogenesis of acne vulgaris. While it is a normal inhabitant of the skin, its overgrowth can lead to inflammation and the formation of acne lesions. The presence of C. acnes triggers an immune response, leading to the recruitment of inflammatory cells and the production of pro-inflammatory cytokines, which exacerbate the condition.
Moreover, the biofilm formation by C. acnes can contribute to chronic inflammation and resistance to treatment. This highlights the importance of targeting this bacterium in acne therapies, particularly with the use of topical and systemic antibiotics that can reduce its population and the associated inflammatory response.
Genetic Predisposition
Genetic factors also play a crucial role in the development of acne vulgaris. Studies have shown that individuals with a family history of acne are more likely to experience the condition themselves. Specific genetic polymorphisms related to sebum production, inflammatory response, and skin barrier function have been identified, suggesting that genetic predisposition may influence the severity and persistence of acne.
Understanding the genetic underpinnings of acne vulgaris can lead to personalized treatment approaches, allowing dermatologists to tailor therapies based on an individual's genetic profile. This emerging field of research holds promise for improving outcomes in acne management.
Clinical Presentation of Acne Vulgaris
Types of Lesions
Acne vulgaris presents with a variety of lesions, which can be classified into non-inflammatory and inflammatory types. Non-inflammatory lesions include open comedones (blackheads) and closed comedones (whiteheads), which are formed when hair follicles become clogged with sebum and dead skin cells. These lesions are often the initial manifestations of acne and can progress to more severe forms if left untreated.
Inflammatory lesions, on the other hand, include papules, pustules, nodules, and cysts. Papules are small, raised, red bumps that indicate inflammation, while pustules are similar but contain pus. Nodules are larger, deeper lesions that can be painful and may lead to scarring, while cysts are large, fluid-filled lesions that can also result in significant scarring. The presence of these inflammatory lesions is often indicative of a more severe form of acne vulgaris, necessitating more aggressive treatment.
Acne Scarring
One of the most concerning aspects of acne vulgaris is the potential for scarring. Acne scars can be classified into atrophic (depressed) and hypertrophic (raised) scars. Atrophic scars, which are the most common, result from the loss of collagen during the healing process and can take various forms, including ice pick, boxcar, and rolling scars. Hypertrophic scars, on the other hand, are raised scars that occur due to excessive collagen production during healing.
Preventing scarring is a critical component of acne management, and early intervention is key. Treatments aimed at reducing inflammation and preventing the formation of new lesions can significantly decrease the risk of scarring. For patients with existing scars, various dermatological procedures, such as chemical peels, laser therapy, and microneedling, may be employed to improve the appearance of the skin.
Diagnosis of Acne Vulgaris
Clinical Evaluation
The diagnosis of acne vulgaris is primarily clinical and is based on the characteristic appearance of the lesions. A thorough history and physical examination are essential for assessing the severity of the condition and determining the appropriate treatment plan. Dermatologists often classify acne severity using grading scales that consider the number and type of lesions present, as well as the impact on the patient's quality of life.
In some cases, additional investigations may be warranted, particularly if there is suspicion of an underlying hormonal disorder or if the acne is resistant to standard treatments. Blood tests to evaluate hormone levels, such as testosterone and insulin, may be conducted to rule out conditions like polycystic ovary syndrome (PCOS) in female patients.
Differential Diagnosis
While acne vulgaris is a common condition, it is essential to differentiate it from other skin disorders that may present with similar lesions. Conditions such as rosacea, folliculitis, and perioral dermatitis can mimic acne and may require different treatment approaches. A thorough understanding of these differential diagnoses is crucial for dermatologists to provide accurate and effective care.
In addition, certain medications and lifestyle factors can exacerbate acne or mimic its presentation. For instance, the use of certain cosmetics, hormonal contraceptives, and medications like corticosteroids can lead to acneiform eruptions. Identifying these contributing factors is vital for developing a comprehensive treatment plan.
Treatment Options for Acne Vulgaris
Topical Treatments
Topical therapies are often the first line of treatment for mild to moderate acne vulgaris. Commonly used topical agents include retinoids, benzoyl peroxide, and topical antibiotics. Retinoids, such as tretinoin and adapalene, work by promoting cell turnover and preventing the formation of comedones. Benzoyl peroxide has antibacterial properties and helps reduce inflammation and sebum production.
Topical antibiotics, such as clindamycin and erythromycin, are effective in reducing the population of C. acnes on the skin. Combination therapies that include both retinoids and benzoyl peroxide or antibiotics are often more effective than monotherapy and are commonly used in clinical practice. Patients should be educated about the potential for skin irritation with these treatments and the importance of gradual introduction to minimize side effects.
Systemic Treatments
For moderate to severe cases of acne vulgaris, systemic treatments may be necessary. Oral antibiotics, such as doxycycline and minocycline, are frequently prescribed to reduce inflammation and bacterial load. These medications are typically used for a limited duration to prevent antibiotic resistance and are often combined with topical therapies for enhanced efficacy.
Hormonal therapies, including oral contraceptives, can be particularly effective in female patients with acne associated with hormonal fluctuations. These medications work by regulating hormone levels and reducing sebum production. In cases of severe, treatment-resistant acne, isotretinoin, a powerful retinoid, may be prescribed. Isotretinoin is highly effective but requires careful monitoring due to its potential side effects, including teratogenicity and effects on liver function.
Physical and Procedural Treatments
In addition to pharmacological therapies, various physical and procedural treatments can be employed to manage acne vulgaris. Chemical peels, which involve the application of chemical agents to exfoliate the skin, can help reduce acne lesions and improve skin texture. Laser therapies, such as fractional laser and blue light therapy, target the sebaceous glands and reduce inflammation, providing effective treatment for acne.
Other procedural options include drainage and extraction of cystic lesions, which can provide immediate relief and prevent scarring. Dermatologists may also recommend microneedling, which promotes collagen production and can improve the appearance of acne scars. These treatments can be particularly beneficial for patients with persistent acne or those seeking to address scarring.
Preventive Measures and Lifestyle Modifications
Skincare Routine
Establishing a proper skincare routine is crucial for managing acne vulgaris. Patients should be encouraged to use non-comedogenic products that do not clog pores and to cleanse the skin gently to avoid irritation. Overwashing or using harsh scrubs can exacerbate acne and lead to increased inflammation. A consistent routine that includes gentle cleansing, moisturizing, and sun protection can help maintain skin health and prevent acne flare-ups.
Additionally, patients should be educated about the importance of avoiding picking or squeezing acne lesions, as this can lead to scarring and further inflammation. Regular follow-up appointments with a dermatologist can help monitor progress and make necessary adjustments to the treatment plan.
Diet and Lifestyle Factors
Emerging evidence suggests that diet and lifestyle factors may play a role in the development and exacerbation of acne vulgaris. High-glycemic index foods, dairy products, and certain dietary patterns have been associated with increased acne severity. Encouraging a balanced diet rich in fruits, vegetables, whole grains, and lean proteins may help improve skin health.
Moreover, stress management techniques, such as mindfulness and regular exercise, can also be beneficial in reducing acne flare-ups. Stress has been shown to influence hormone levels and may exacerbate acne, making it essential for patients to adopt healthy coping mechanisms.
Conclusion
Acne vulgaris is a complex dermatological condition that requires a comprehensive understanding of its pathophysiology, clinical presentation, and treatment options. By recognizing the multifactorial nature of acne and employing a combination of topical, systemic, and procedural therapies, dermatologists can effectively manage this condition and improve the quality of life for affected individuals. Ongoing research into the genetic, hormonal, and environmental factors influencing acne will continue to enhance our understanding and treatment of this common skin disorder.
Visit Our Offices
Services:
- • Medical Dermatology
- • Surgical Dermatology
- • Laser Treatments
- • Cosmetic Dermatology
Services:
- • Medical Dermatology
- • Surgical Dermatology
- • Laser Treatments
- • Cosmetic Dermatology
Visit Our Offices
Services:
- • Medical Dermatology
- • Surgical Dermatology
- • Laser Treatments
- • Cosmetic Dermatology
Services:
- • Medical Dermatology
- • Surgical Dermatology
- • Laser Treatments
- • Cosmetic Dermatology