Introduction to Acne Scarring
Acne scarring is a common consequence of acne vulgaris, a skin condition that affects millions of individuals worldwide. The formation of scars occurs as a result of the skin's healing process following the inflammation caused by acne lesions. Understanding the pathophysiology of acne scarring is crucial for both prevention and treatment. This glossary entry aims to provide a comprehensive overview of acne scarring, including its types, causes, treatment options, and preventive measures.
Acne itself can manifest in various forms, including comedones (blackheads and whiteheads), papules, pustules, nodules, and cysts. Each of these types can lead to different forms of scarring, depending on the severity of the acne and the individual's skin type. The scars left behind can significantly impact a person's self-esteem and quality of life, making it essential to address both the acne and its aftermath effectively.
Types of Acne Scars
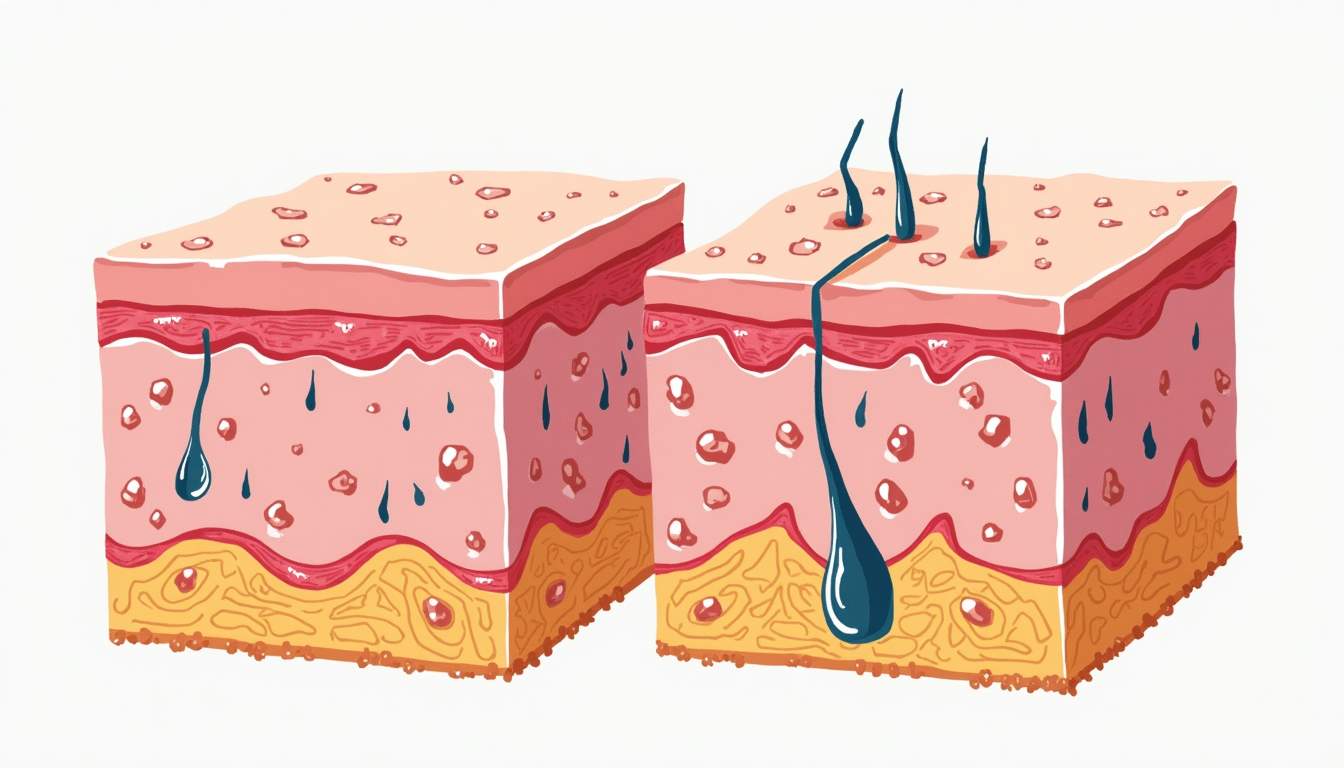
Acne scars can generally be categorized into two main types: atrophic scars and hypertrophic scars. Each type has distinct characteristics and requires different approaches for treatment.
Atrophic Scars
Atrophic scars are the most common type of acne scars and are characterized by a loss of tissue. These scars typically appear as depressions or indentations in the skin. They can be further classified into three subtypes:
- Ice Pick Scars: These are narrow, deep scars that resemble small punctures in the skin. They are often the result of cystic acne and can be challenging to treat due to their depth.
- Boxcar Scars: Boxcar scars are wider than ice pick scars and have sharp, defined edges. They usually occur in areas where acne lesions were more severe, leading to significant tissue loss.
- Rolling Scars: Rolling scars have a wave-like appearance and are caused by the fibrous bands of tissue that form beneath the skin. They create an uneven texture and can be more challenging to treat than other types of atrophic scars.
Hypertrophic Scars
Hypertrophic scars, in contrast to atrophic scars, are raised scars that occur when the body produces too much collagen during the healing process. These scars can be red or darker than the surrounding skin and may become itchy or painful. They are more common in individuals with darker skin tones and can be particularly distressing due to their prominent appearance.
Causes of Acne Scarring
The development of acne scars is influenced by several factors, including the severity of the acne, the type of lesions, and individual skin characteristics. Understanding these causes is essential for effective prevention and treatment.
Severity of Acne
Severe forms of acne, such as cystic acne, are more likely to result in scarring. The deeper the acne lesion penetrates into the skin, the greater the likelihood of tissue damage and subsequent scarring. Individuals with mild acne may experience some degree of scarring, but it is generally less pronounced than in those with severe forms.
Inflammation and Infection
Inflammation plays a critical role in the formation of acne scars. When acne lesions become inflamed, the body responds by sending immune cells to the affected area, which can lead to tissue damage. Additionally, if acne lesions become infected, the risk of scarring increases as the body attempts to heal the damaged tissue.
Skin Type and Genetics
Individual skin characteristics, including skin type and genetic predisposition, can also influence the likelihood of developing acne scars. Individuals with oily skin may be more prone to developing acne, while those with darker skin tones may be at a higher risk for hypertrophic scars due to increased melanin production during the healing process. Genetics can also play a role, as some individuals may have a hereditary tendency to scar more easily than others.
Treatment Options for Acne Scarring
There are various treatment options available for acne scarring, ranging from topical treatments to more invasive procedures. The choice of treatment depends on the type and severity of the scars, as well as the individual's skin type and preferences.
Topical Treatments
Topical treatments are often the first line of defense against acne scarring. These treatments can help improve skin texture and reduce the appearance of scars over time. Common topical treatments include:
- Retinoids: These vitamin A derivatives promote cell turnover and can help fade hyperpigmentation associated with acne scars.
- Alpha Hydroxy Acids (AHAs): AHAs, such as glycolic acid, exfoliate the skin and can improve the appearance of superficial scars.
- Beta Hydroxy Acids (BHAs): Salicylic acid is a BHA that can penetrate deep into the pores and help reduce inflammation, preventing further scarring.
Procedural Treatments
For more severe scarring, procedural treatments may be necessary. These treatments are typically performed by dermatologists and can provide more significant results than topical treatments alone. Common procedural treatments include:
- Laser Therapy: Laser treatments can target the deeper layers of skin, promoting collagen production and improving skin texture.
- Microneedling: This procedure involves using fine needles to create micro-injuries in the skin, stimulating the body's natural healing process and collagen production.
- Chemical Peels: Chemical peels involve applying a solution to the skin that exfoliates the top layers, revealing smoother skin underneath.
- Dermal Fillers: Fillers can be injected into atrophic scars to raise them to the level of the surrounding skin, improving overall texture.
Preventive Measures
Preventing acne scarring begins with effective acne management. By addressing acne early and properly, individuals can significantly reduce their risk of developing scars. Here are some preventive measures:
Proper Acne Treatment
Using appropriate acne treatments, such as topical retinoids, benzoyl peroxide, and antibiotics, can help control breakouts and minimize inflammation. It is essential to consult a dermatologist for personalized treatment plans tailored to individual skin types and acne severity.
Avoid Picking or Squeezing Lesions
One of the most critical preventive measures is to avoid picking, squeezing, or popping acne lesions. This can lead to further inflammation, infection, and ultimately, scarring. Educating patients about the importance of leaving lesions alone can help reduce the risk of scarring.
Sun Protection
Sun exposure can exacerbate the appearance of scars, making them more noticeable. Using broad-spectrum sunscreen with an SPF of 30 or higher can help protect the skin and prevent hyperpigmentation associated with scars. Wearing protective clothing and seeking shade during peak sun hours are additional measures to consider.
Conclusion
Acne scarring is a multifaceted issue that can significantly affect an individual's self-esteem and quality of life. Understanding the types, causes, and treatment options for acne scars is essential for effective management. By employing preventive measures and seeking appropriate treatments, individuals can minimize the impact of acne scarring and achieve healthier, clearer skin.
As research in dermatology continues to evolve, new treatment modalities and techniques are being developed to address acne scarring more effectively. Staying informed about advancements in dermatological care can empower individuals to make educated decisions regarding their skin health.
Visit Our Offices
Services:
- • Medical Dermatology
- • Surgical Dermatology
- • Laser Treatments
- • Cosmetic Dermatology
Services:
- • Medical Dermatology
- • Surgical Dermatology
- • Laser Treatments
- • Cosmetic Dermatology
Visit Our Offices
Services:
- • Medical Dermatology
- • Surgical Dermatology
- • Laser Treatments
- • Cosmetic Dermatology
Services:
- • Medical Dermatology
- • Surgical Dermatology
- • Laser Treatments
- • Cosmetic Dermatology