Introduction to Trichoscopy
Trichoscopy is a specialized dermatological technique that involves the examination of hair and scalp using a dermatoscope, a handheld device that magnifies and illuminates the skin. This non-invasive method allows dermatologists to observe hair follicles and scalp conditions in detail, aiding in the diagnosis and management of various hair disorders. Trichoscopy is particularly valuable because it provides insights into the morphology of hair and scalp, which are often not visible to the naked eye.
The term 'trichoscopy' is derived from the Greek words 'trichos,' meaning hair, and 'skopein,' meaning to look or examine. This technique has gained prominence in recent years due to its ability to enhance the diagnostic accuracy for conditions such as alopecia, scalp psoriasis, and seborrheic dermatitis. By utilizing trichoscopy, dermatologists can differentiate between various types of hair loss and scalp diseases, leading to more effective treatment plans.
In this glossary entry, we will explore the various aspects of trichoscopy, including its history, techniques, applications, and the common conditions it helps to diagnose. We will also discuss the advantages and limitations of trichoscopy in dermatology.
History of Trichoscopy
The roots of trichoscopy can be traced back to the early 20th century, when dermatologists began to recognize the importance of examining hair and scalp disorders in a more detailed manner. The advent of the dermatoscope, initially designed for skin examinations, paved the way for the development of trichoscopy as a distinct field. Early practitioners utilized simple magnifying lenses to observe hair and scalp conditions, but these methods were limited in their effectiveness.
In the 1990s, advancements in dermatoscopic technology led to the formalization of trichoscopy as a diagnostic tool. Researchers and dermatologists began to publish findings on the specific patterns and features observed in hair and scalp disorders, establishing a foundation for the systematic use of trichoscopy in clinical practice. The introduction of digital dermatoscopes further enhanced the capabilities of trichoscopy, allowing for high-resolution imaging and the ability to document findings for further analysis.
Today, trichoscopy is recognized as an essential component of dermatological practice, with numerous studies validating its effectiveness in diagnosing hair and scalp conditions. The technique continues to evolve, with ongoing research aimed at refining its applications and improving diagnostic accuracy.
Techniques Used in Trichoscopy
Dermatoscopic Examination
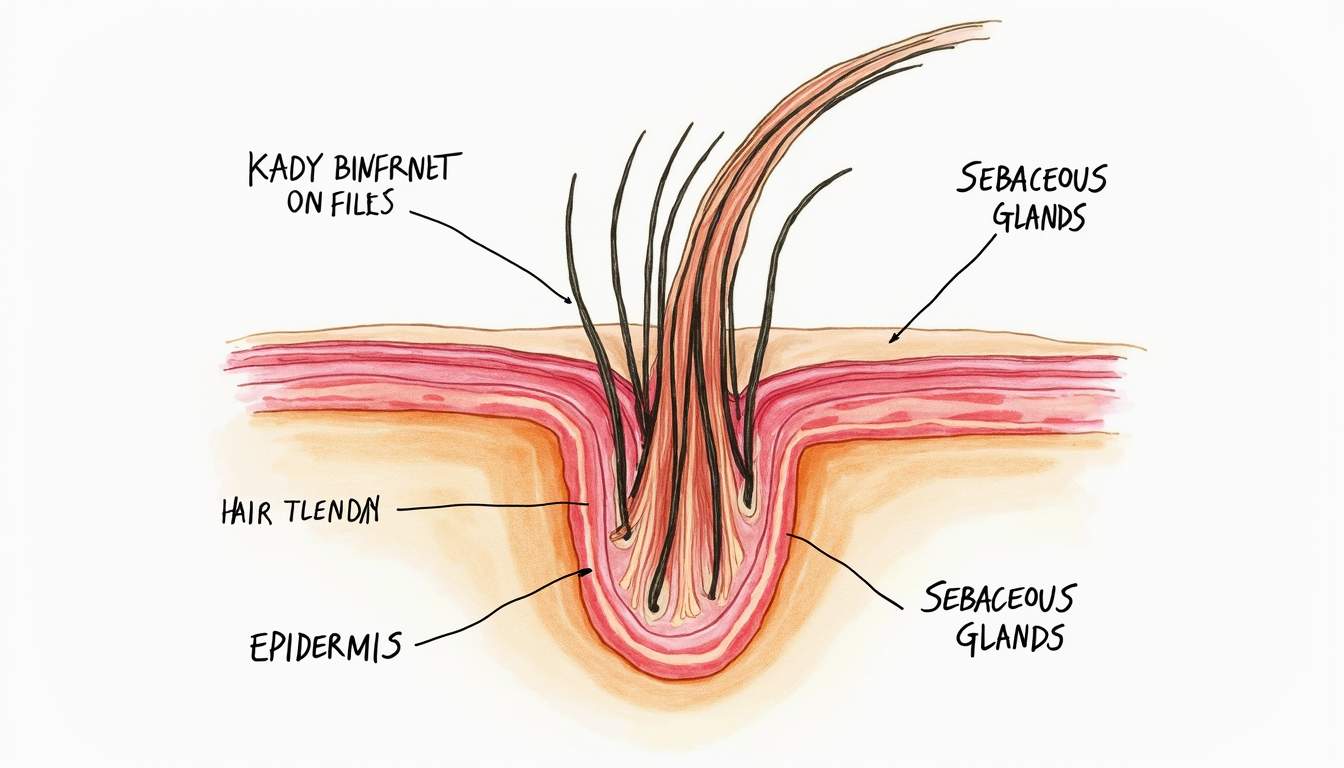
The primary technique used in trichoscopy is dermatoscopic examination, which involves the use of a dermatoscope to visualize the hair and scalp. The dermatoscope typically consists of a magnifying lens, a light source, and a transparent plate that allows for direct contact with the skin. This setup enables the dermatologist to observe the hair follicles, scalp surface, and any associated lesions in high detail.
During a dermatoscopic examination, the dermatologist will systematically assess the scalp and hair, looking for specific patterns, colors, and structures. Common features examined include hair shaft thickness, follicular openings, and the presence of any inflammatory changes. The examination may be performed in various lighting conditions, including polarized light, which can enhance the visibility of certain features.
Digital Trichoscopy
Digital trichoscopy is an advanced form of trichoscopy that utilizes digital imaging technology to capture high-resolution images of the scalp and hair. This technique allows for detailed documentation of findings, which can be invaluable for tracking disease progression and treatment response over time. Digital trichoscopy can also facilitate teledermatology, enabling dermatologists to consult with patients remotely.
In digital trichoscopy, images can be analyzed using specialized software that highlights specific features and patterns. This analysis can assist in the identification of various hair disorders, as well as in the development of personalized treatment plans. The ability to store and compare images over time enhances the overall diagnostic process and provides a comprehensive view of the patient's condition.
Applications of Trichoscopy
Diagnosis of Hair Loss Disorders
One of the primary applications of trichoscopy is in the diagnosis of hair loss disorders, such as androgenetic alopecia, alopecia areata, and telogen effluvium. Each of these conditions presents with distinct dermatoscopic features that can aid in accurate diagnosis. For example, in androgenetic alopecia, trichoscopy may reveal miniaturized hair follicles and a characteristic pattern of hair thinning, while alopecia areata may show exclamation mark hairs and a loss of pigmentation around the follicles.
By utilizing trichoscopy, dermatologists can differentiate between these conditions and determine the most appropriate treatment options. This is particularly important, as the management of hair loss disorders can vary significantly based on the underlying cause. Accurate diagnosis through trichoscopy can lead to timely interventions and improved patient outcomes.
Assessment of Scalp Conditions
Trichoscopy is also valuable in assessing various scalp conditions, including seborrheic dermatitis, psoriasis, and folliculitis. Each of these conditions presents unique dermatoscopic findings that can help dermatologists establish a diagnosis. For instance, seborrheic dermatitis may show greasy scales and inflammation around hair follicles, while psoriasis may present with well-defined red plaques and silvery scales.
By examining these features through trichoscopy, dermatologists can gain insights into the severity of the condition and tailor treatment strategies accordingly. This is particularly important for chronic scalp conditions, where ongoing management may be necessary to control symptoms and prevent flare-ups.
Common Conditions Diagnosed with Trichoscopy
Alopecia Areata
Alopecia areata is an autoimmune condition characterized by sudden hair loss in patches. Trichoscopy can reveal specific features such as exclamation mark hairs, which are short, broken hairs that taper at the base, and yellow dots, which represent keratin debris in the hair follicles. These findings can help confirm the diagnosis and differentiate alopecia areata from other forms of hair loss.
Androgenetic Alopecia
Androgenetic alopecia, commonly known as male or female pattern baldness, is a hereditary condition that leads to progressive hair thinning. Trichoscopy can demonstrate miniaturization of hair follicles, a reduction in hair density, and a characteristic pattern of hair loss. These features are crucial for diagnosing androgenetic alopecia and determining the appropriate treatment, which may include topical minoxidil or oral finasteride.
Telogen Effluvium
Telogen effluvium is a temporary form of hair loss that often occurs after stress, illness, or hormonal changes. Trichoscopy can reveal an increased number of telogen hairs, which are in the resting phase of the hair growth cycle. Identifying these features can help dermatologists reassure patients about the transient nature of the condition and guide them toward appropriate management strategies.
Advantages of Trichoscopy
Trichoscopy offers several advantages over traditional diagnostic methods for hair and scalp disorders. Firstly, it is a non-invasive technique that does not require any skin biopsies or invasive procedures, making it more comfortable for patients. Secondly, trichoscopy provides real-time visualization of hair and scalp features, allowing for immediate diagnosis and treatment planning.
Additionally, the ability to document findings through digital trichoscopy enhances the overall diagnostic process. Dermatologists can track changes over time, assess treatment efficacy, and make informed decisions based on objective data. This is particularly beneficial for chronic conditions that require ongoing management and monitoring.
Limitations of Trichoscopy
Despite its many advantages, trichoscopy does have some limitations. One significant limitation is that it requires a trained dermatologist to interpret the findings accurately. The subjective nature of dermatoscopic examination means that the accuracy of diagnosis can vary depending on the clinician's experience and expertise.
Furthermore, while trichoscopy can provide valuable insights into hair and scalp conditions, it may not always be sufficient for a definitive diagnosis. In some cases, additional tests, such as scalp biopsies or blood tests, may be necessary to confirm a diagnosis or rule out underlying systemic conditions.
Conclusion
In summary, trichoscopy is a vital tool in the field of dermatology that enhances the diagnosis and management of hair and scalp disorders. By utilizing advanced dermatoscopic techniques, dermatologists can gain valuable insights into the morphology of hair and scalp conditions, leading to more accurate diagnoses and effective treatment plans. As the field of trichoscopy continues to evolve, ongoing research and technological advancements will likely further enhance its applications and improve patient outcomes.
For patients experiencing hair or scalp issues, consulting with a dermatologist who is skilled in trichoscopy can provide a comprehensive evaluation and tailored management strategies. With its non-invasive nature and ability to provide detailed insights, trichoscopy represents a significant advancement in dermatological practice.
Visit Our Offices
Services:
- • Medical Dermatology
- • Surgical Dermatology
- • Laser Treatments
- • Cosmetic Dermatology
Services:
- • Medical Dermatology
- • Surgical Dermatology
- • Laser Treatments
- • Cosmetic Dermatology
Visit Our Offices
Services:
- • Medical Dermatology
- • Surgical Dermatology
- • Laser Treatments
- • Cosmetic Dermatology
Services:
- • Medical Dermatology
- • Surgical Dermatology
- • Laser Treatments
- • Cosmetic Dermatology