Introduction to Squamous Cell Carcinoma
Squamous Cell Carcinoma (SCC) is a type of skin cancer that arises from the squamous cells, which are flat cells located in the outer layer of the skin, known as the epidermis. It is one of the most common forms of skin cancer, alongside basal cell carcinoma (BCC) and melanoma. SCC typically develops in areas of the skin that have been exposed to the sun, such as the face, ears, neck, and hands, but it can also occur in other parts of the body, including mucous membranes and internal organs.
The incidence of SCC has been rising in recent years, largely due to increased sun exposure, tanning bed use, and the aging population. While SCC is generally considered less aggressive than melanoma, it can still be serious and may metastasize (spread) to other parts of the body if left untreated. Early detection and treatment are crucial for improving outcomes and minimizing the risk of complications.
Understanding the characteristics, risk factors, symptoms, diagnosis, treatment options, and prevention strategies associated with SCC is essential for both patients and healthcare providers. This glossary entry aims to provide a comprehensive overview of these aspects, contributing to a better understanding of this prevalent dermatological condition.
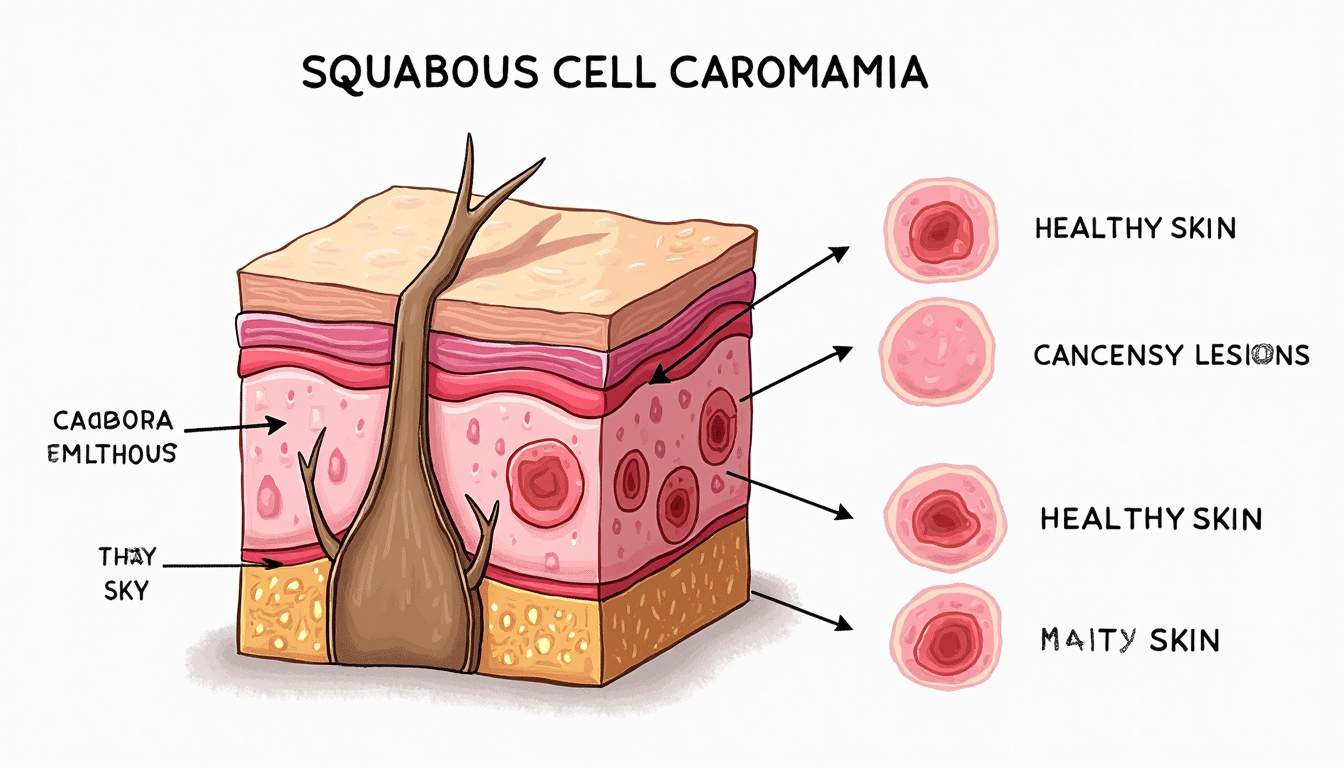
Characteristics of Squamous Cell Carcinoma
Histopathology
Histopathologically, squamous cell carcinoma is characterized by the abnormal proliferation of squamous cells. These cells may exhibit atypical features, including enlarged nuclei, increased mitotic activity, and keratinization. SCC can be classified into various subtypes based on the degree of differentiation, which refers to how much the cancer cells resemble normal squamous cells. Well-differentiated SCC tends to grow more slowly and has a better prognosis, while poorly differentiated SCC is more aggressive and has a higher potential for metastasis.
Microscopically, SCC may present as a keratinizing or non-keratinizing tumor, with keratin pearls being a common feature in well-differentiated forms. The tumor may invade the surrounding dermis and can be associated with a desmoplastic stroma, which is a fibrous tissue response to the tumor. The presence of inflammatory infiltrates and necrosis may also be observed in more aggressive forms of SCC.
In addition to the histological features, SCC can also be classified based on its clinical presentation, which may include nodular, ulcerative, or infiltrative forms. The clinical appearance of SCC can vary significantly, making it essential for dermatologists to conduct thorough examinations and consider differential diagnoses when evaluating suspicious lesions.
Clinical Presentation
The clinical presentation of squamous cell carcinoma can vary widely, but it typically manifests as a persistent, non-healing sore, a scaly patch, or a wart-like growth. These lesions may be red, crusted, or ulcerated, and they often bleed or become painful. In some cases, SCC may present as a keratotic lesion, which is characterized by a thickened, rough surface. It is important to note that SCC can sometimes mimic benign skin conditions, such as actinic keratosis or basal cell carcinoma, making accurate diagnosis challenging.
Patients may also report symptoms such as itching, tenderness, or discomfort in the affected area. The lesions can occur on sun-exposed areas, but they can also arise in areas that are not typically exposed to sunlight, particularly in individuals with immunosuppression or chronic inflammation. The variability in presentation underscores the importance of regular skin examinations and prompt evaluation of any new or changing lesions.
In advanced cases, SCC can lead to significant morbidity, including local tissue destruction, disfigurement, and functional impairment, particularly when the tumor invades deeper structures such as cartilage or bone. Therefore, timely recognition and treatment are critical to preventing these complications.
Risk Factors for Squamous Cell Carcinoma
Environmental Factors
Environmental factors play a significant role in the development of squamous cell carcinoma. The most well-established risk factor is ultraviolet (UV) radiation exposure, primarily from the sun. Chronic sun exposure leads to cumulative DNA damage in skin cells, increasing the likelihood of malignant transformation. Individuals who spend prolonged periods outdoors, such as farmers, construction workers, and outdoor athletes, are at a higher risk for developing SCC.
Additionally, the use of tanning beds, which emit concentrated UV radiation, has been linked to an increased risk of SCC, particularly among younger individuals. Other environmental factors that may contribute to the development of SCC include exposure to certain chemicals, such as arsenic, coal tar, and industrial oils, as well as radiation exposure from previous cancer treatments.
Genetic and Biological Factors
Genetic predisposition also plays a role in the risk of developing squamous cell carcinoma. Individuals with a family history of skin cancer or genetic syndromes such as xeroderma pigmentosum or albinism are at an increased risk due to their impaired ability to repair DNA damage caused by UV exposure. Furthermore, individuals with fair skin, light hair, and light-colored eyes are more susceptible to SCC due to lower levels of melanin, which provides some protection against UV radiation.
Other biological factors that may increase the risk of SCC include immunosuppression, whether due to organ transplantation, HIV infection, or the use of immunosuppressive medications. These individuals are at a significantly higher risk of developing skin cancers, including SCC, due to their compromised immune response, which is less capable of identifying and eliminating malignant cells.
Diagnosis of Squamous Cell Carcinoma
Clinical Examination
The diagnosis of squamous cell carcinoma begins with a thorough clinical examination by a dermatologist. During this examination, the physician will assess the patient's medical history, including any previous skin cancers, sun exposure history, and risk factors. The dermatologist will then perform a physical examination of the skin, looking for suspicious lesions that may warrant further investigation.
During the examination, the dermatologist will evaluate the characteristics of any lesions, including size, shape, color, texture, and the presence of symptoms such as bleeding or pain. If a lesion appears suspicious, the dermatologist may recommend a biopsy to confirm the diagnosis. It is essential for healthcare providers to be vigilant in recognizing the clinical features of SCC, as early detection is key to successful treatment.
Biopsy and Histopathological Analysis
A biopsy is the definitive method for diagnosing squamous cell carcinoma. There are several types of biopsies that may be performed, including shave biopsy, punch biopsy, and excisional biopsy, depending on the size and location of the lesion. The chosen method will allow for the collection of tissue samples that can be examined microscopically for the presence of malignant squamous cells.
Once the biopsy is performed, the tissue sample is sent to a pathology laboratory, where a pathologist will conduct a histopathological analysis. This analysis involves examining the tissue under a microscope to identify any abnormal cellular features consistent with SCC. The pathologist will also assess the degree of differentiation of the tumor and may provide information on the tumor's depth of invasion and other histological characteristics that can influence treatment decisions.
Treatment Options for Squamous Cell Carcinoma
Non-Surgical Treatments
Non-surgical treatment options for squamous cell carcinoma may be appropriate for superficial lesions or for patients who are not candidates for surgery due to health concerns. These treatments may include topical chemotherapy, photodynamic therapy, and cryotherapy. Topical chemotherapy involves the application of chemotherapeutic agents directly to the skin lesion, which can help to destroy cancerous cells. Common agents used include 5-fluorouracil and imiquimod.
Photodynamic therapy (PDT) is another non-invasive treatment option that utilizes a photosensitizing agent and light exposure to selectively destroy cancer cells. This method is particularly effective for superficial SCC and actinic keratosis. Cryotherapy involves freezing the cancerous lesion with liquid nitrogen, causing cell death and subsequent shedding of the affected skin.
Surgical Treatments
Surgical excision remains the primary treatment for squamous cell carcinoma, particularly for invasive lesions. The goal of surgery is to completely remove the tumor along with a margin of healthy tissue to minimize the risk of recurrence. Mohs micrographic surgery is a specialized technique that is often employed for SCC located in cosmetically sensitive areas, such as the face. This technique involves the stepwise removal of the tumor and immediate microscopic examination of the excised tissue to ensure complete removal while preserving as much surrounding healthy tissue as possible.
In cases where SCC has metastasized or is locally advanced, additional treatments such as radiation therapy or systemic therapies may be indicated. Radiation therapy can be used as an adjunct to surgery or as a primary treatment for patients who are not surgical candidates. Systemic therapies, including targeted therapies and immunotherapy, are being explored for advanced SCC, particularly in cases where the cancer has spread beyond the skin.
Prevention Strategies for Squamous Cell Carcinoma
Sun Protection Measures
Preventing squamous cell carcinoma primarily involves minimizing UV radiation exposure. Effective sun protection measures include wearing broad-spectrum sunscreen with a high SPF, seeking shade during peak sun hours, and wearing protective clothing, such as wide-brimmed hats and long-sleeved shirts. Sunscreen should be applied generously and reapplied every two hours, especially after swimming or sweating.
Additionally, avoiding tanning beds and educating individuals about the dangers of UV exposure are critical components of prevention strategies. Public health campaigns aimed at raising awareness about the risks of skin cancer and promoting sun safety can significantly reduce the incidence of SCC and other skin cancers.
Regular Skin Examinations
Regular skin examinations are essential for early detection of squamous cell carcinoma. Individuals, especially those at higher risk, should perform self-examinations of their skin monthly to identify any new or changing lesions. Dermatologists recommend annual skin checks for individuals with a history of skin cancer, significant sun exposure, or other risk factors. Early detection through routine examinations can lead to timely intervention and improved outcomes.
In conclusion, squamous cell carcinoma is a common skin cancer with distinct characteristics, risk factors, and treatment options. Understanding the nature of SCC, recognizing its clinical presentation, and implementing preventive measures are crucial for reducing its incidence and improving patient outcomes. Ongoing research and advancements in dermatology continue to enhance our understanding of SCC, paving the way for more effective prevention and treatment strategies.
Visit Our Offices
Services:
- • Medical Dermatology
- • Surgical Dermatology
- • Laser Treatments
- • Cosmetic Dermatology
Services:
- • Medical Dermatology
- • Surgical Dermatology
- • Laser Treatments
- • Cosmetic Dermatology
Visit Our Offices
Services:
- • Medical Dermatology
- • Surgical Dermatology
- • Laser Treatments
- • Cosmetic Dermatology
Services:
- • Medical Dermatology
- • Surgical Dermatology
- • Laser Treatments
- • Cosmetic Dermatology