Introduction to Non-Melanoma Skin Cancer
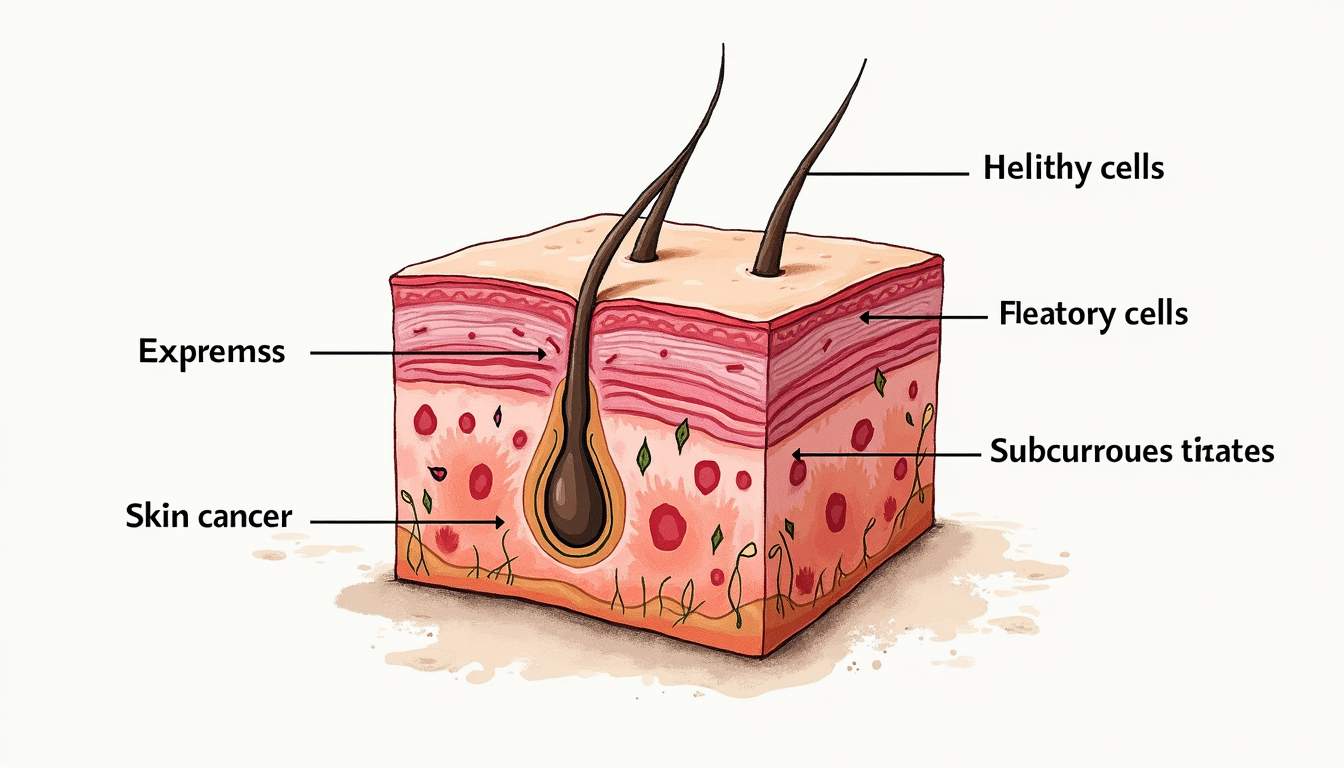
Non-melanoma skin cancer (NMSC) refers to a group of cancers that develop in the skin's outer layer, primarily affecting the epidermis. Unlike melanoma, which arises from melanocytes (the pigment-producing cells), non-melanoma skin cancers typically originate from keratinocytes, the predominant cells in the epidermis. The two most common types of NMSC are basal cell carcinoma (BCC) and squamous cell carcinoma (SCC). Understanding these cancers is crucial for effective prevention, early detection, and treatment.
The incidence of non-melanoma skin cancer has been rising globally, largely due to increased sun exposure and the aging population. Although NMSC is generally less aggressive than melanoma, it can still lead to significant morbidity and, in rare cases, mortality if left untreated. This glossary aims to provide a comprehensive overview of non-melanoma skin cancer, including its types, risk factors, symptoms, diagnosis, treatment options, and prevention strategies.
Types of Non-Melanoma Skin Cancer
Basal Cell Carcinoma (BCC)
Basal cell carcinoma is the most prevalent form of skin cancer, accounting for approximately 80% of all non-melanoma skin cancers. BCC arises from the basal cells located in the lower part of the epidermis. It is characterized by slow growth and rarely metastasizes to other parts of the body. BCC typically appears as a pearly or waxy bump, a flat, flesh-colored lesion, or a scar-like area on sun-exposed skin.
There are several subtypes of basal cell carcinoma, including:
- Nodular BCC: The most common subtype, presenting as a raised, dome-shaped bump.
- Superficial BCC: Appears as a red, scaly patch that may bleed or crust.
- Morfeiform BCC: Resembles a scar and can be more aggressive, often requiring more extensive treatment.
- Infiltrative BCC: Grows deeper into the skin and can be challenging to treat due to its indistinct borders.
Squamous Cell Carcinoma (SCC)
Squamous cell carcinoma is the second most common type of non-melanoma skin cancer, arising from squamous cells in the epidermis. SCC can occur on any part of the body but is most frequently found on sun-exposed areas such as the face, ears, neck, and back of the hands. Unlike BCC, SCC has a higher potential to metastasize, making early detection and treatment essential.
Common characteristics of squamous cell carcinoma include:
- Firm, red nodules: Often with a scaly or crusted surface.
- Flat lesions: These may appear as scaly patches that can bleed or ulcerate.
- Keratoacanthoma: A variant of SCC that can resemble a rapidly growing tumor but is often self-limiting.
Risk Factors for Non-Melanoma Skin Cancer
Understanding the risk factors associated with non-melanoma skin cancer is vital for prevention and early detection. The following factors have been identified as significant contributors to the development of NMSC:
Ultraviolet (UV) Radiation Exposure
One of the most significant risk factors for non-melanoma skin cancer is exposure to ultraviolet (UV) radiation from the sun or artificial sources such as tanning beds. UV radiation damages the DNA in skin cells, leading to mutations that can result in cancer. Individuals who spend prolonged periods outdoors without adequate sun protection are at a higher risk.
Skin Type and Color
Individuals with fair skin, light-colored eyes, and red or blonde hair are at a greater risk of developing non-melanoma skin cancer. This is due to lower levels of melanin, which provides some protection against UV radiation. People with darker skin tones can also develop NMSC, but the incidence is generally lower.
Age and Gender
Age is another critical factor, as the risk of developing non-melanoma skin cancer increases with advancing age. This is partly due to cumulative sun exposure over a lifetime. Additionally, men are more likely to develop NMSC than women, possibly due to greater occupational sun exposure and differences in sun protection behaviors.
Immune System Suppression
Individuals with weakened immune systems, such as organ transplant recipients or those with certain autoimmune diseases, are at an increased risk of developing non-melanoma skin cancer. The immune system plays a crucial role in detecting and destroying cancerous cells, and its suppression can lead to an increased likelihood of tumor formation.
Symptoms of Non-Melanoma Skin Cancer
Recognizing the symptoms of non-melanoma skin cancer is essential for early diagnosis and treatment. The symptoms can vary depending on the type of cancer, but common signs include:
Changes in Skin Appearance
Individuals may notice new growths or changes in existing moles or spots on their skin. Basal cell carcinoma often appears as a shiny, pearly bump or a flat, scaly patch, while squamous cell carcinoma may present as a firm, red nodule or a scaly lesion. Any persistent changes in the skin's appearance should be evaluated by a healthcare professional.
Bleeding or Crusting
Non-melanoma skin cancers can sometimes bleed, crust, or ulcerate. If a lesion does not heal or continues to bleed, it is essential to seek medical advice. These symptoms may indicate a more aggressive form of cancer that requires prompt intervention.
Itching or Pain
Some individuals may experience itching, tenderness, or pain in the affected area. While these symptoms can be associated with various skin conditions, persistent discomfort should not be ignored, as it may indicate the presence of skin cancer.
Diagnosis of Non-Melanoma Skin Cancer
Diagnosing non-melanoma skin cancer typically involves a thorough examination by a dermatologist, who will assess the skin for any suspicious lesions. If skin cancer is suspected, the following diagnostic procedures may be employed:
Skin Examination
A comprehensive skin examination is the first step in diagnosing non-melanoma skin cancer. The dermatologist will inspect the skin for any unusual growths, changes in existing moles, or other concerning features. This examination may include the use of a dermatoscope, a specialized tool that allows for a closer look at the skin's surface.
Biopsy
If a suspicious lesion is identified, a biopsy may be performed to confirm the diagnosis. During a biopsy, a small sample of skin is removed and sent to a laboratory for analysis. There are several types of biopsies, including:
- Shave biopsy: A thin layer of skin is shaved off the surface.
- Excisional biopsy: The entire lesion is removed along with a margin of surrounding tissue.
- Incisional biopsy: A portion of the lesion is removed for examination.
Treatment Options for Non-Melanoma Skin Cancer
Treatment for non-melanoma skin cancer depends on several factors, including the type, size, location, and depth of the cancer, as well as the patient's overall health. Common treatment options include:
Topical Treatments
For superficial basal cell carcinomas and some squamous cell carcinomas, topical chemotherapy agents such as 5-fluorouracil (5-FU) or imiquimod may be prescribed. These medications are applied directly to the skin and work by destroying cancerous cells. Topical treatments are often preferred for patients who are not candidates for surgery or who have multiple lesions.
Surgical Excision
Surgical excision is a common treatment for non-melanoma skin cancer, particularly for larger or deeper lesions. During this procedure, the cancerous tissue is removed along with a margin of healthy skin to ensure complete removal. The excised area is then closed with sutures. This method is effective for both BCC and SCC and has a high cure rate.
Mohs Micrographic Surgery
Mohs micrographic surgery is a specialized surgical technique used primarily for non-melanoma skin cancers located in cosmetically sensitive areas, such as the face. This technique involves the stepwise removal of cancerous tissue, with immediate microscopic examination of the margins. If cancerous cells are detected at the margins, additional layers are removed until clear margins are achieved. Mohs surgery offers the highest cure rates and minimizes the risk of scarring.
Radiation Therapy
Radiation therapy may be recommended for patients who are not surgical candidates or for those with non-melanoma skin cancers that are difficult to treat surgically. This treatment uses high-energy rays to target and kill cancer cells. Radiation therapy can be effective for certain types of SCC and BCC, particularly in older patients or those with multiple lesions.
Prevention of Non-Melanoma Skin Cancer
Preventing non-melanoma skin cancer is largely centered around minimizing UV exposure and adopting sun-safe behaviors. Here are several effective strategies:
Sun Protection
Using broad-spectrum sunscreen with an SPF of 30 or higher is crucial for protecting the skin from harmful UV rays. Sunscreen should be applied generously and reapplied every two hours, especially after swimming or sweating. Additionally, wearing protective clothing, such as long sleeves and wide-brimmed hats, can further reduce UV exposure.
Avoiding Tanning Beds
Artificial tanning devices, such as tanning beds and booths, emit UV radiation that can significantly increase the risk of developing non-melanoma skin cancer. It is advisable to avoid these devices altogether and opt for safer alternatives, such as self-tanning lotions or sprays.
Regular Skin Checks
Regular self-examinations of the skin can help individuals detect any changes early. It is essential to be aware of the ABCDEs of melanoma (Asymmetry, Border, Color, Diameter, Evolving) and to consult a dermatologist for any suspicious lesions. Additionally, professional skin examinations by a dermatologist should be conducted annually, especially for those at higher risk.
Conclusion
Non-melanoma skin cancer represents a significant public health concern, given its increasing incidence and potential for morbidity. Understanding the types, risk factors, symptoms, diagnosis, treatment options, and prevention strategies associated with NMSC is crucial for effective management. By adopting sun-safe practices and seeking regular skin evaluations, individuals can significantly reduce their risk of developing non-melanoma skin cancer and ensure early detection and treatment when necessary.
Visit Our Offices
Services:
- • Medical Dermatology
- • Surgical Dermatology
- • Laser Treatments
- • Cosmetic Dermatology
Services:
- • Medical Dermatology
- • Surgical Dermatology
- • Laser Treatments
- • Cosmetic Dermatology
Visit Our Offices
Services:
- • Medical Dermatology
- • Surgical Dermatology
- • Laser Treatments
- • Cosmetic Dermatology
Services:
- • Medical Dermatology
- • Surgical Dermatology
- • Laser Treatments
- • Cosmetic Dermatology