Introduction to Skin Grafting
Skin grafting is a surgical procedure that involves the transplantation of skin from one area of the body (the donor site) to another area (the recipient site) to cover wounds, burns, or defects. This technique is widely used in dermatology to promote healing, restore skin integrity, and improve the aesthetic appearance of the affected area. The necessity for skin grafting arises from various conditions, including traumatic injuries, surgical excisions, chronic ulcers, and congenital defects.
The procedure can be categorized into different types based on the source of the graft, the thickness of the skin being grafted, and the method of application. Understanding the intricacies of skin grafting is essential for both healthcare professionals and patients, as it plays a critical role in wound management and reconstructive surgery.
This glossary entry will delve into the various aspects of skin grafting, including its types, indications, techniques, complications, and post-operative care, providing a comprehensive overview for those seeking knowledge in the field of dermatology.
Types of Skin Grafts
Skin grafts can be classified into several categories based on their origin and structure. The primary types of skin grafts include:
- Autografts: These are grafts taken from the patient's own body, typically from areas that are not affected by the injury or disease. Autografts are preferred due to their lower risk of rejection and complications.
- Allografts: These grafts are obtained from a donor of the same species, usually from deceased individuals. Allografts are often used temporarily to cover wounds until the patient's own skin can regenerate.
- Xenografts: These grafts are derived from a different species, such as pigs. Xenografts are primarily used for temporary coverage and are not meant for permanent use.
In addition to these classifications, skin grafts can also be categorized based on their thickness:
- Split-thickness grafts: These grafts consist of the epidermis and a portion of the dermis. They are commonly used for larger wounds and can be harvested from various body sites.
- Full-thickness grafts: These grafts include the entire epidermis and dermis. They are typically used for smaller areas that require better cosmetic results, such as the face or hands.
Indications for Skin Grafting
Skin grafting is indicated in a variety of clinical situations. Some of the most common indications include:
- Burns: Severe burns, particularly third-degree burns, often require skin grafting to promote healing and restore skin integrity.
- Traumatic injuries: Skin grafting is frequently used to treat traumatic wounds resulting from accidents, animal bites, or surgical excisions.
- Chronic ulcers: Non-healing ulcers, such as diabetic foot ulcers or venous stasis ulcers, may necessitate skin grafting to facilitate healing.
- Congenital defects: Conditions such as cleft lip and palate or other congenital skin defects may require grafting for reconstruction.
In addition to these conditions, skin grafting may also be employed in cosmetic procedures, such as scar revision or to improve the appearance of skin after tumor excision.
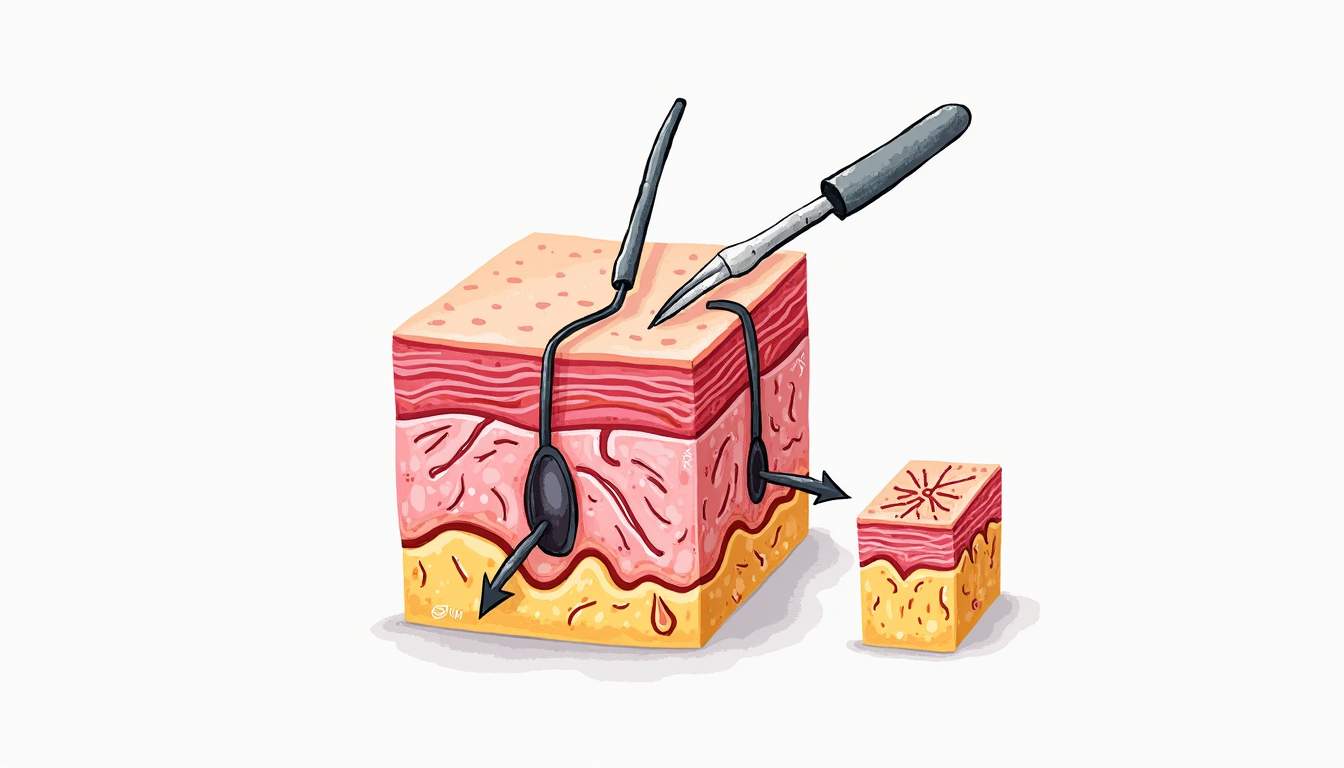
Techniques of Skin Grafting
The technique for performing a skin graft can vary based on the type of graft being used and the specific requirements of the patient. The general steps involved in skin grafting include:
Preparation of the Recipient Site
The recipient site must be adequately prepared to ensure optimal healing. This may involve debridement of necrotic tissue, cleaning the wound, and ensuring that the area is free of infection. In some cases, the recipient site may need to be vascularized to promote graft survival.
Harvesting the Graft
The harvesting of the graft is a critical step in the procedure. For autografts, the surgeon will select a donor site, typically an area with healthy skin, such as the thigh or abdomen. The skin is then carefully excised using a scalpel or dermatome, ensuring that the graft maintains its integrity and is of appropriate size for the recipient site.
Application of the Graft
Once the graft is harvested, it is placed onto the recipient site. The graft must be positioned correctly to ensure proper adherence and to minimize the risk of complications. The surgeon may use sutures, staples, or adhesive dressings to secure the graft in place. It is crucial to avoid any tension on the graft, as this can lead to complications such as necrosis or poor healing.
Post-operative Care
Post-operative care is essential for the success of the skin graft. Patients are typically advised to keep the graft site clean and dry, and to follow specific instructions regarding dressing changes. Pain management and monitoring for signs of infection are also critical components of post-operative care. Follow-up appointments are necessary to assess graft viability and healing progress.
Complications of Skin Grafting
While skin grafting is generally a safe procedure, it is not without potential complications. Some of the most common complications include:
- Graft failure: This occurs when the graft does not adhere properly to the recipient site or becomes necrotic due to inadequate blood supply.
- Infection: The risk of infection is present in any surgical procedure, and infections can compromise the success of the graft.
- Scarring: Scarring at both the donor and recipient sites is a common outcome of skin grafting, and the extent of scarring can vary based on individual healing responses.
- Contractures: In some cases, the skin may heal in a contracted manner, leading to restricted movement or deformity.
It is essential for patients to be aware of these potential complications and to communicate with their healthcare providers regarding any concerns during the recovery process.
Conclusion
Skin grafting is a vital technique in dermatology that plays a significant role in wound healing and skin restoration. Understanding the types, indications, techniques, and potential complications of skin grafting can empower patients and healthcare professionals alike. As advancements in surgical techniques and wound care continue to evolve, the outcomes of skin grafting are expected to improve, offering hope and healing to those in need.
For individuals considering skin grafting, it is crucial to consult with a qualified dermatologist or plastic surgeon who can provide personalized recommendations based on the specific circumstances and needs of the patient. With appropriate care and management, skin grafting can lead to successful outcomes and enhanced quality of life.
Visit Our Offices
Services:
- • Medical Dermatology
- • Surgical Dermatology
- • Laser Treatments
- • Cosmetic Dermatology
Services:
- • Medical Dermatology
- • Surgical Dermatology
- • Laser Treatments
- • Cosmetic Dermatology
Visit Our Offices
Services:
- • Medical Dermatology
- • Surgical Dermatology
- • Laser Treatments
- • Cosmetic Dermatology
Services:
- • Medical Dermatology
- • Surgical Dermatology
- • Laser Treatments
- • Cosmetic Dermatology