Introduction to Wound Healing
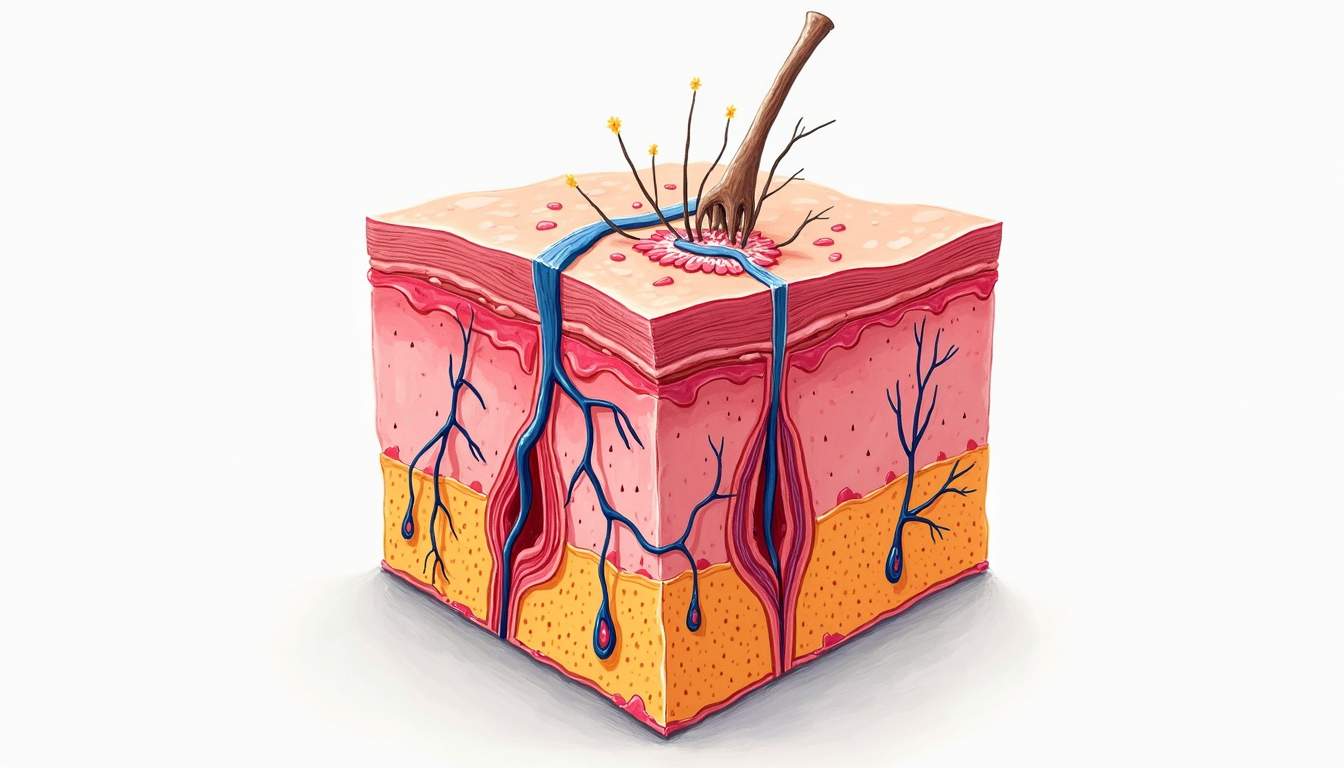
Wound healing is a complex biological process that involves a series of coordinated events aimed at restoring the integrity of the skin and underlying tissues following injury. This process is crucial not only for physical recovery but also for the prevention of infections and other complications that can arise from skin breaches. In dermatology, understanding the mechanisms of wound healing is essential for effective treatment and management of various skin conditions, including ulcers, surgical wounds, and traumatic injuries.
The wound healing process can be broadly categorized into four overlapping phases: hemostasis, inflammation, proliferation, and remodeling. Each of these phases plays a vital role in ensuring that the wound heals properly and efficiently. The duration and effectiveness of each phase can be influenced by various factors, including the type of wound, the patient's overall health, and external environmental conditions.
In this glossary entry, we will explore the intricacies of wound healing, including the phases involved, the cellular and molecular mechanisms at play, factors that can affect healing, and common wound healing disorders. This comprehensive understanding is essential for dermatologists and healthcare professionals involved in wound care.
Phases of Wound Healing
1. Hemostasis
The initial phase of wound healing, hemostasis, begins immediately after injury. This phase is characterized by the rapid constriction of blood vessels to minimize blood loss, followed by the aggregation of platelets to form a temporary clot. The clot serves as a physical barrier to pathogens and provides a scaffold for incoming cells involved in the healing process.
During hemostasis, platelets release various growth factors and cytokines that initiate the inflammatory response. These signaling molecules play a crucial role in attracting immune cells to the site of injury, setting the stage for the subsequent inflammatory phase. The importance of hemostasis cannot be overstated, as inadequate clot formation can lead to excessive bleeding and delayed healing.
2. Inflammation
The inflammatory phase typically begins within hours of injury and can last for several days. During this phase, immune cells, particularly neutrophils and macrophages, migrate to the wound site. Neutrophils are the first responders, working to clear debris and pathogens through phagocytosis. Following this, macrophages take over, playing a dual role in both clearing debris and releasing cytokines that promote healing.
Macrophages are essential for transitioning the wound from the inflammatory phase to the proliferative phase. They secrete growth factors such as Transforming Growth Factor-beta (TGF-β) and Vascular Endothelial Growth Factor (VEGF), which stimulate angiogenesis (the formation of new blood vessels) and fibroblast proliferation. The inflammatory phase is characterized by redness, swelling, heat, and pain, which are all signs of the body's immune response to injury.
3. Proliferation
The proliferative phase generally occurs between days 3 and 21 post-injury and is marked by tissue formation and repair. During this phase, fibroblasts play a central role by synthesizing collagen and extracellular matrix components, which provide structural support to the newly formed tissue. This is also the phase where angiogenesis occurs, ensuring that the new tissue receives adequate blood supply.
In addition to fibroblasts, keratinocytes migrate across the wound bed to re-establish the epidermal barrier. This migration is crucial for protecting the underlying tissues and preventing infection. The formation of granulation tissue, which is rich in collagen, blood vessels, and inflammatory cells, is a hallmark of this phase. As the wound continues to heal, myofibroblasts appear, which help contract the wound and reduce its size.
4. Remodeling
The remodeling phase can last for months to years, depending on the severity of the wound. During this phase, the collagen matrix undergoes reorganization and maturation, leading to increased tensile strength of the healed tissue. Type III collagen, which is initially laid down during the proliferative phase, is gradually replaced by stronger Type I collagen.
Throughout the remodeling phase, the wound continues to gain strength, although it may never return to its original state. The final scar tissue is often less vascularized and has a different texture compared to the surrounding skin. Factors such as age, nutrition, and underlying health conditions can significantly influence the remodeling process and the final appearance of the scar.
Cellular and Molecular Mechanisms in Wound Healing
Growth Factors
Growth factors are critical signaling molecules that orchestrate the wound healing process. They are involved in various stages, including cell proliferation, migration, and differentiation. Key growth factors include Platelet-Derived Growth Factor (PDGF), Epidermal Growth Factor (EGF), and Fibroblast Growth Factor (FGF). Each of these factors has specific roles in promoting healing and tissue regeneration.
For instance, PDGF is released by platelets during hemostasis and is crucial for attracting fibroblasts and smooth muscle cells to the wound site. EGF stimulates keratinocyte proliferation and migration, which is essential for re-epithelialization. FGF plays a significant role in angiogenesis, ensuring that the newly formed tissue receives adequate blood supply. Understanding the roles of these growth factors can help in developing targeted therapies to enhance wound healing.
Extracellular Matrix (ECM)
The extracellular matrix (ECM) is a complex network of proteins and carbohydrates that provides structural and biochemical support to surrounding cells. In wound healing, the ECM serves as a scaffold for cell attachment and migration, facilitating the repair process. Components of the ECM, such as collagen, elastin, and glycosaminoglycans, play vital roles in maintaining tissue integrity and function.
During the proliferative phase, fibroblasts synthesize new ECM components, which are crucial for forming granulation tissue. The composition and organization of the ECM can significantly influence the healing process, as it affects cell behavior and the overall mechanical properties of the tissue. Disruptions in ECM production or remodeling can lead to chronic wounds or abnormal scarring, such as hypertrophic scars or keloids.
Factors Affecting Wound Healing
Patient-Related Factors
Several patient-related factors can significantly influence the wound healing process. Age is one of the most critical factors, as older adults often experience delayed healing due to reduced cellular proliferation and impaired immune response. Chronic conditions such as diabetes mellitus can also impede healing by affecting blood flow and increasing the risk of infection.
Nutrition plays a vital role in wound healing, as adequate protein intake is essential for collagen synthesis and tissue repair. Micronutrients such as vitamin C, zinc, and vitamin A are also important for various aspects of the healing process. Additionally, lifestyle factors such as smoking and alcohol consumption can negatively impact wound healing by impairing blood flow and immune function.
Environmental Factors
Environmental factors, including moisture, temperature, and oxygen levels, can also affect wound healing. Maintaining an optimal moisture balance is crucial, as both excessive dryness and excessive moisture can hinder healing. Temperature plays a role in cellular metabolism, with warmer temperatures generally promoting faster healing.
Oxygen is essential for cellular respiration and the production of energy required for the healing process. Hypoxia (low oxygen levels) can lead to impaired healing and increased risk of infection. Therefore, ensuring adequate oxygenation of the wound is vital, particularly in cases of chronic wounds or in patients with compromised circulation.
Common Wound Healing Disorders
Chronic Wounds
Chronic wounds are defined as wounds that fail to progress through the normal stages of healing and persist for an extended period, typically longer than three months. Common types of chronic wounds include diabetic ulcers, venous ulcers, and pressure ulcers. These wounds often result from a combination of factors, including poor circulation, infection, and underlying health conditions.
Managing chronic wounds requires a multidisciplinary approach, including wound care specialists, nutritionists, and physical therapists. Treatment may involve debridement (removal of dead tissue), advanced dressings, and sometimes surgical interventions to promote healing. Understanding the underlying causes of chronic wounds is essential for developing effective treatment plans.
Hypertrophic Scars and Keloids
Hypertrophic scars and keloids are abnormal forms of scarring that can occur following wound healing. Hypertrophic scars are raised, red scars that remain confined to the boundaries of the original wound, often improving over time. In contrast, keloids extend beyond the original wound site and can be larger than the initial injury. Keloids are often itchy or painful and can be challenging to treat.
Both hypertrophic scars and keloids result from an overproduction of collagen during the remodeling phase of wound healing. Treatment options include corticosteroid injections, silicone gel sheets, and in some cases, surgical excision. Understanding the mechanisms behind these abnormal scars can help in developing preventive strategies and effective treatments.
Conclusion
Wound healing is a multifaceted process that involves a series of complex biological events aimed at restoring tissue integrity following injury. Understanding the phases of wound healing, the cellular and molecular mechanisms involved, and the factors that can influence healing is essential for effective management of wounds in dermatology. Additionally, recognizing common wound healing disorders and their treatment options is crucial for healthcare professionals working in this field.
As research continues to advance our understanding of wound healing, new therapeutic approaches and technologies are being developed to enhance healing outcomes and improve the quality of life for patients with wounds. By integrating this knowledge into clinical practice, dermatologists and healthcare providers can better support their patients in achieving optimal wound healing.
Visit Our Offices
Services:
- • Medical Dermatology
- • Surgical Dermatology
- • Laser Treatments
- • Cosmetic Dermatology
Services:
- • Medical Dermatology
- • Surgical Dermatology
- • Laser Treatments
- • Cosmetic Dermatology
Visit Our Offices
Services:
- • Medical Dermatology
- • Surgical Dermatology
- • Laser Treatments
- • Cosmetic Dermatology
Services:
- • Medical Dermatology
- • Surgical Dermatology
- • Laser Treatments
- • Cosmetic Dermatology