Introduction to Vasodilation
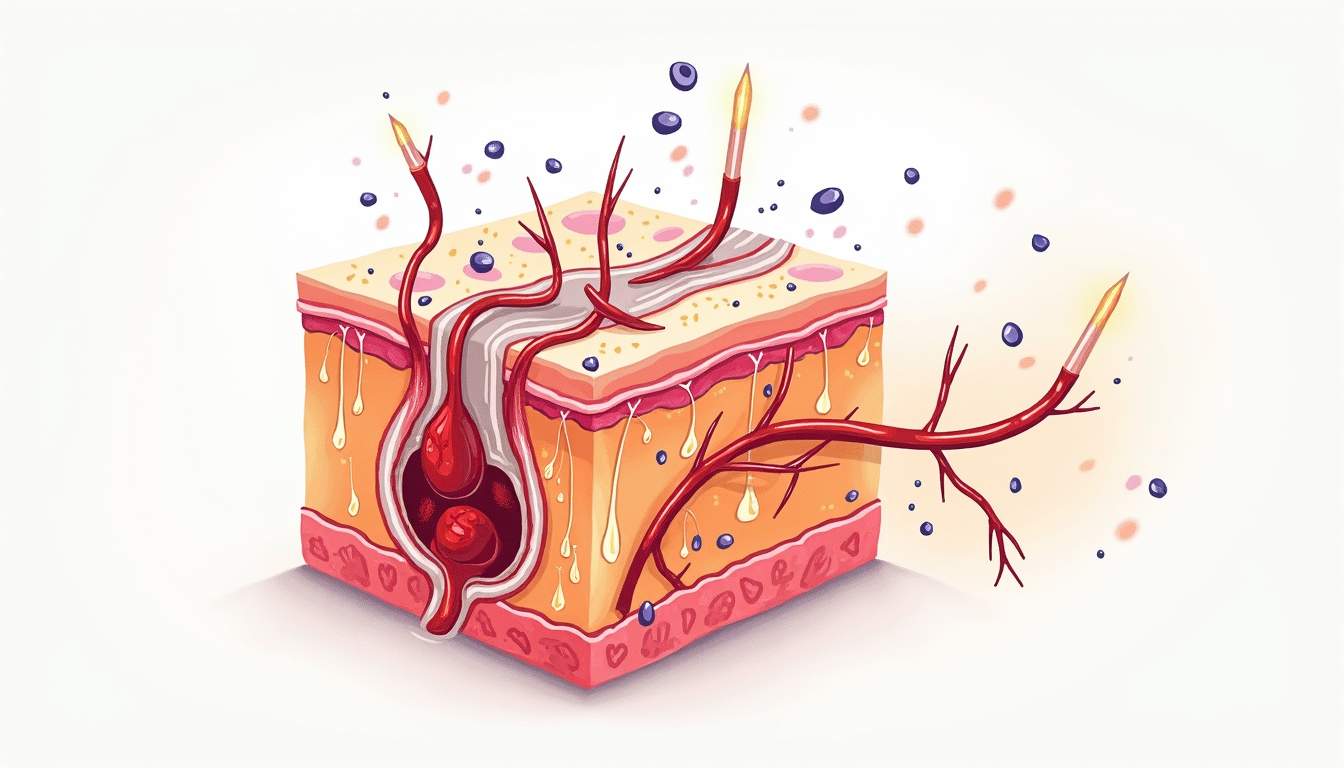
Vasodilation is a physiological process characterized by the widening of blood vessels, particularly the arteries and arterioles. This widening occurs due to the relaxation of smooth muscle cells within the vessel walls, leading to an increase in blood flow to various tissues, including the skin. In dermatology, understanding vasodilation is crucial as it plays a significant role in various skin conditions, inflammatory responses, and the overall health of the skin.
The process of vasodilation is regulated by several factors, including neural, hormonal, and local biochemical signals. These factors work in concert to ensure that blood flow is appropriately adjusted according to the body's needs, such as during exercise, heat exposure, or in response to injury. In dermatology, vasodilation is particularly relevant in the context of skin flushing, erythema, and the pathophysiology of various dermatological disorders.
In this glossary entry, we will explore the mechanisms of vasodilation, its significance in dermatology, the conditions associated with abnormal vasodilation, and the therapeutic implications of modulating this process in skin health.
Mechanisms of Vasodilation
Physiological Mechanisms
Vasodilation is primarily mediated by the relaxation of vascular smooth muscle cells, which is influenced by several physiological mechanisms. One of the most significant mediators of vasodilation is nitric oxide (NO), a gas produced by endothelial cells lining the blood vessels. When endothelial cells are stimulated by various factors, such as shear stress from blood flow or inflammatory cytokines, they release NO, which diffuses into the smooth muscle cells and activates guanylate cyclase. This enzyme increases the levels of cyclic guanosine monophosphate (cGMP), leading to muscle relaxation and subsequent vasodilation.
Another important mechanism involves the role of prostaglandins, which are lipid compounds derived from arachidonic acid. Prostaglandins, particularly prostaglandin E2 (PGE2), can induce vasodilation by acting on specific receptors on smooth muscle cells, leading to increased intracellular cAMP levels and relaxation of the muscle. Additionally, bradykinin, a peptide that promotes vasodilation, is released during inflammatory responses and can enhance blood flow to affected areas, contributing to the redness and warmth associated with inflammation.
Furthermore, the autonomic nervous system plays a critical role in regulating vasodilation. The sympathetic nervous system typically induces vasoconstriction, while the parasympathetic nervous system promotes vasodilation through the release of acetylcholine, which can stimulate endothelial cells to produce NO. This balance between sympathetic and parasympathetic activity is essential for maintaining proper blood flow and pressure throughout the body.
Local Factors Influencing Vasodilation
In addition to systemic mechanisms, local factors within the skin can significantly influence vasodilation. For instance, during physical activity or exposure to heat, local temperature increases can lead to vasodilation as the body attempts to dissipate heat through increased blood flow to the skin. This process is mediated by thermoreceptors that signal the hypothalamus to initiate vasodilation in peripheral blood vessels.
Moreover, inflammatory mediators released during skin injury or infection, such as histamine, can cause localized vasodilation. Histamine is released by mast cells and plays a pivotal role in allergic reactions and inflammatory responses. It binds to H1 receptors on endothelial cells, leading to increased permeability and vasodilation, which results in the characteristic swelling and redness of inflamed skin.
Other local factors include the presence of certain metabolites, such as carbon dioxide and lactic acid, which accumulate in tissues during metabolic activity. These metabolites can induce vasodilation by signaling to smooth muscle cells to relax, thereby increasing blood flow to meet the metabolic demands of the tissue.
Significance of Vasodilation in Dermatology
Role in Skin Health
Vasodilation plays a crucial role in maintaining skin health by ensuring adequate blood supply to the dermis, where essential nutrients, oxygen, and immune cells are delivered. This blood flow is vital for the repair and regeneration of skin tissues, particularly after injury or in response to environmental stressors. Furthermore, vasodilation facilitates the removal of metabolic waste products from the skin, contributing to overall skin homeostasis.
In addition to its role in nutrient delivery, vasodilation is essential for thermoregulation. The skin acts as a major organ for heat dissipation, and vasodilation allows for increased blood flow to the skin surface, where heat can be released into the environment. This process is particularly important during exercise or in hot conditions, as it helps to prevent overheating and maintain core body temperature.
Moreover, vasodilation is involved in the inflammatory response, which is a critical aspect of skin health. When the skin is injured or infected, vasodilation facilitates the influx of immune cells to the affected area, promoting healing and defense against pathogens. However, excessive or prolonged vasodilation can lead to chronic inflammation and contribute to various dermatological conditions.
Conditions Associated with Abnormal Vasodilation
Abnormal vasodilation can manifest in various dermatological conditions, leading to symptoms such as erythema, flushing, and telangiectasia. One common condition associated with abnormal vasodilation is rosacea, a chronic inflammatory skin disorder characterized by facial redness, flushing, and visible blood vessels. In rosacea, there is a dysregulation of the vascular response, leading to excessive vasodilation and increased sensitivity to triggers such as heat, alcohol, and spicy foods.
Another condition linked to abnormal vasodilation is psoriasis, an autoimmune skin disorder that can present with red, scaly plaques. In psoriasis, inflammatory mediators promote vasodilation and increase blood flow to the affected areas, contributing to the erythematous appearance of the lesions. Understanding the role of vasodilation in psoriasis has led to the development of targeted therapies aimed at modulating the inflammatory response and restoring normal vascular function.
Additionally, conditions such as systemic lupus erythematosus (SLE) and scleroderma can also involve abnormal vasodilation. In SLE, vasodilation can lead to skin rashes and photosensitivity, while in scleroderma, there may be an initial phase of vasodilation followed by vascular damage and subsequent vasoconstriction, resulting in skin thickening and fibrosis.
Therapeutic Implications of Vasodilation in Dermatology
Pharmacological Interventions
Understanding the mechanisms of vasodilation has significant therapeutic implications in dermatology. Pharmacological agents that target vasodilation can be used to manage various skin conditions. For instance, topical and systemic medications that enhance nitric oxide production or mimic its effects can be employed to treat conditions characterized by inadequate blood flow or excessive vasoconstriction.
One such class of medications is phosphodiesterase inhibitors, which prevent the breakdown of cGMP, thereby promoting vasodilation. These agents can be beneficial in treating conditions like erectile dysfunction and pulmonary hypertension, and their potential applications in dermatology are being explored, particularly in enhancing blood flow to the skin and improving wound healing.
Additionally, anti-inflammatory medications that modulate the vascular response, such as corticosteroids, can be used to reduce excessive vasodilation associated with inflammatory skin conditions. By controlling inflammation and vascular permeability, these medications can alleviate symptoms and promote healing in conditions like eczema and dermatitis.
Non-Pharmacological Approaches
In addition to pharmacological interventions, non-pharmacological approaches can also influence vasodilation and improve skin health. Lifestyle modifications, such as regular exercise, can enhance vascular function and promote healthy blood flow to the skin. Exercise-induced vasodilation not only improves nutrient delivery but also stimulates the release of beneficial hormones and growth factors that support skin health.
Furthermore, dietary factors can play a role in modulating vasodilation. Consuming foods rich in antioxidants, omega-3 fatty acids, and flavonoids can promote endothelial health and enhance the body's ability to regulate blood flow. Hydration is also crucial, as adequate fluid intake supports optimal blood volume and circulation, contributing to healthy skin.
Lastly, stress management techniques, such as mindfulness and relaxation exercises, can help regulate the autonomic nervous system and promote a balanced vascular response. Chronic stress can lead to dysregulation of vasodilation, contributing to skin issues such as acne and eczema. By addressing stress, individuals can improve their skin health and overall well-being.
Conclusion
Vasodilation is a fundamental physiological process with significant implications for dermatology. Understanding the mechanisms of vasodilation, its role in skin health, and the conditions associated with abnormal vasodilation is essential for dermatologists and healthcare providers. By leveraging both pharmacological and non-pharmacological approaches, it is possible to modulate vasodilation and improve skin health outcomes for patients. As research continues to evolve, new therapeutic strategies targeting vasodilation may emerge, offering hope for individuals affected by various dermatological conditions.
Visit Our Offices
Services:
- • Medical Dermatology
- • Surgical Dermatology
- • Laser Treatments
- • Cosmetic Dermatology
Services:
- • Medical Dermatology
- • Surgical Dermatology
- • Laser Treatments
- • Cosmetic Dermatology
Visit Our Offices
Services:
- • Medical Dermatology
- • Surgical Dermatology
- • Laser Treatments
- • Cosmetic Dermatology
Services:
- • Medical Dermatology
- • Surgical Dermatology
- • Laser Treatments
- • Cosmetic Dermatology