Introduction to Transdermal Delivery
Transdermal delivery refers to the method of administering medication through the skin for systemic effects. This innovative approach bypasses the gastrointestinal tract and hepatic first-pass metabolism, allowing for more efficient absorption of drugs into the bloodstream. The skin, being the largest organ of the human body, serves as a barrier that can be manipulated to enhance drug delivery. This method is particularly significant in dermatology, where localized treatments can be effectively administered while minimizing systemic side effects.
In dermatology, transdermal delivery systems are utilized for a variety of therapeutic purposes, including pain management, hormone replacement therapy, and the treatment of chronic skin conditions. The development of transdermal patches, gels, and creams has revolutionized the way dermatological medications are delivered, providing patients with more convenient and effective treatment options.
Understanding the mechanisms, advantages, and challenges of transdermal delivery is crucial for both healthcare professionals and patients. This glossary entry aims to provide a comprehensive overview of transdermal delivery in the context of dermatology, exploring its applications, formulations, and future directions.
Mechanisms of Transdermal Drug Delivery
Skin Structure and Function
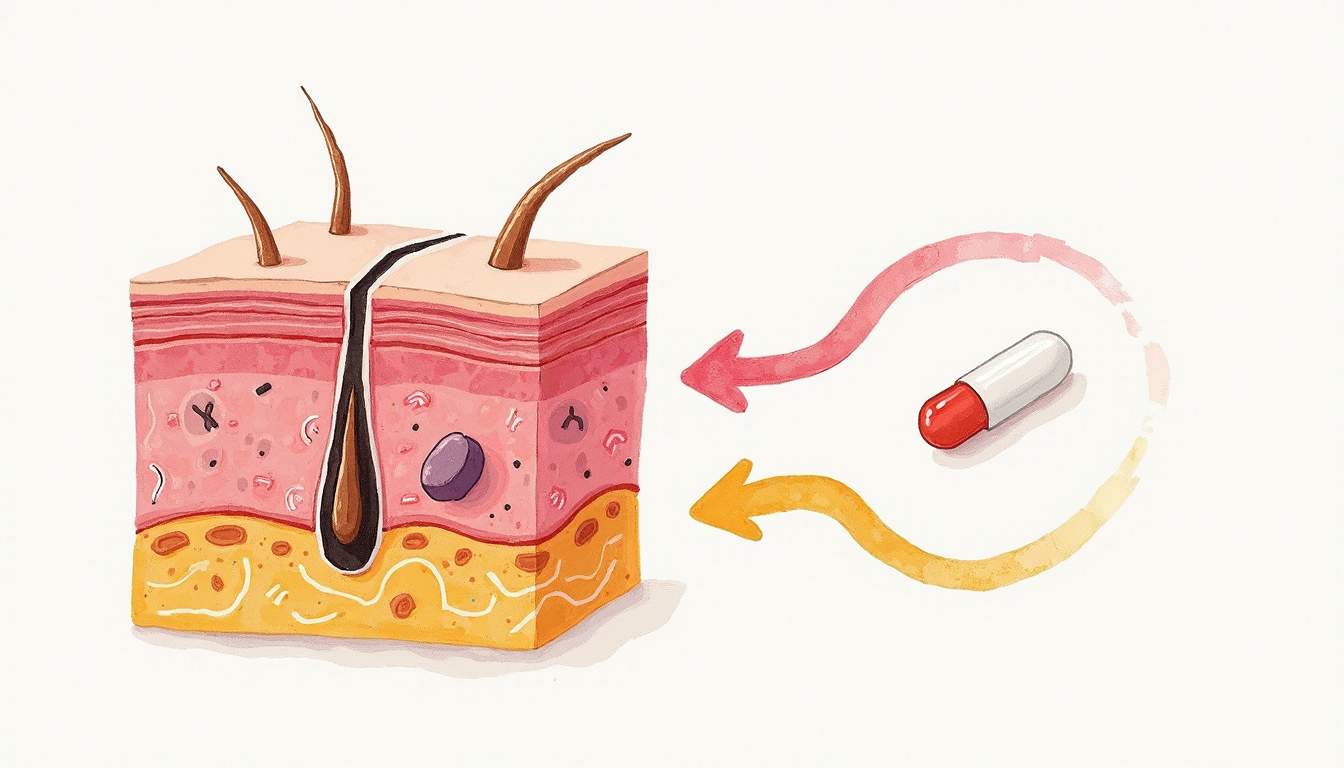
The skin is composed of three primary layers: the epidermis, dermis, and subcutaneous tissue. The outermost layer, the epidermis, acts as a barrier to protect the underlying tissues from environmental factors, pathogens, and chemical substances. Within the epidermis, the stratum corneum (the outermost layer) plays a critical role in transdermal drug delivery, as it is the primary barrier that drugs must penetrate to reach systemic circulation.
The dermis, located beneath the epidermis, contains blood vessels, lymphatics, and nerve endings. It provides structural support and nourishment to the epidermis. The subcutaneous tissue, or hypodermis, consists of fat and connective tissue that insulates the body and serves as an energy reserve. Understanding the anatomy and physiology of these layers is essential for developing effective transdermal delivery systems.
Drug Penetration Pathways
Drugs can penetrate the skin through various pathways, including transcellular (through cells), intercellular (between cells), and appendageal (through hair follicles and sweat glands). The transcellular route involves the drug diffusing through the lipid bilayers of the skin cells, while the intercellular route allows the drug to move through the lipid matrix that surrounds the cells. The appendageal route, although less significant, can also contribute to drug absorption, particularly for larger molecules.
Each of these pathways presents unique challenges and opportunities for drug formulation. For instance, lipophilic (fat-soluble) drugs may favor the transcellular route, while hydrophilic (water-soluble) drugs may benefit from the intercellular pathway. Formulators must consider these factors when designing transdermal delivery systems to optimize drug absorption and efficacy.
Types of Transdermal Delivery Systems
Transdermal Patches
Transdermal patches are adhesive devices that deliver a specific dose of medication through the skin over an extended period. These patches are designed to release the drug at a controlled rate, ensuring a steady concentration in the bloodstream. They are commonly used for hormone replacement therapy, nicotine cessation, and pain management.
There are several types of transdermal patches, including matrix patches, reservoir patches, and microemulsion patches. Matrix patches contain the drug dispersed within a polymer matrix, while reservoir patches have a separate drug reservoir that allows for more precise control over drug release. Microemulsion patches utilize a combination of water and oil to enhance drug solubility and skin penetration.
Topical Gels and Creams
Topical gels and creams are semi-solid formulations that can also be used for transdermal delivery. These formulations often contain penetration enhancers, which are substances that temporarily disrupt the skin barrier to facilitate drug absorption. Gels typically have a higher water content, making them suitable for hydrophilic drugs, while creams are emulsions that can accommodate both hydrophilic and lipophilic drugs.
Formulating effective topical gels and creams requires a careful balance of excipients, active ingredients, and penetration enhancers to ensure optimal drug delivery. The choice of formulation can significantly impact the therapeutic outcomes, making it essential for dermatologists and pharmacists to understand the properties of these products.
Advantages of Transdermal Delivery
Transdermal delivery offers several advantages over traditional oral or injectable routes of administration. One of the most significant benefits is the avoidance of first-pass metabolism, which can significantly reduce the bioavailability of certain drugs when taken orally. By delivering medications directly through the skin, transdermal systems can achieve higher plasma concentrations and more consistent therapeutic effects.
Additionally, transdermal delivery provides a non-invasive and convenient method for patients. Patches, gels, and creams can be easily applied and removed, allowing for flexible dosing schedules. This convenience can improve patient adherence to treatment regimens, particularly for chronic conditions that require long-term therapy.
Moreover, transdermal systems can minimize gastrointestinal side effects and reduce the risk of infections associated with injections. This makes transdermal delivery an attractive option for patients who may be needle-averse or have difficulty swallowing pills.
Challenges in Transdermal Delivery
Despite its many advantages, transdermal delivery also presents several challenges. One of the primary limitations is the skin's barrier function, which can restrict the absorption of larger molecules and hydrophilic drugs. This necessitates the use of penetration enhancers or advanced drug delivery technologies to improve drug permeability.
Another challenge is the variability in skin permeability among individuals, which can be influenced by factors such as age, skin condition, and hydration levels. This variability can lead to inconsistent drug absorption and therapeutic outcomes, making it essential for healthcare providers to monitor patients closely and adjust treatment plans as needed.
Furthermore, the formulation of transdermal systems must consider factors such as stability, compatibility of ingredients, and patient comfort. Ensuring that the formulation remains effective over time while being well-tolerated by the skin is crucial for the success of transdermal delivery systems.
Future Directions in Transdermal Drug Delivery
The field of transdermal drug delivery is continually evolving, with ongoing research focused on improving drug formulations and delivery technologies. Innovations such as microneedles, which create microchannels in the skin to enhance drug penetration, hold promise for delivering larger molecules, including vaccines and biologics.
Additionally, advancements in nanotechnology are paving the way for the development of nanoparticles and liposomes that can encapsulate drugs and facilitate their transport across the skin barrier. These technologies may significantly enhance the efficacy of transdermal delivery systems, allowing for more effective treatment options for patients.
As the demand for non-invasive drug delivery methods continues to grow, the future of transdermal delivery in dermatology looks promising. Ongoing research and development will likely lead to new formulations and technologies that can address current challenges and improve patient outcomes.
Conclusion
Transdermal delivery represents a significant advancement in the field of dermatology, providing a versatile and effective method for administering medications. By understanding the mechanisms, types, advantages, and challenges of transdermal delivery, healthcare professionals can better utilize these systems to enhance patient care. As research continues to advance, the potential for transdermal delivery to revolutionize the treatment of various dermatological conditions remains substantial.
Visit Our Offices
Services:
- • Medical Dermatology
- • Surgical Dermatology
- • Laser Treatments
- • Cosmetic Dermatology
Services:
- • Medical Dermatology
- • Surgical Dermatology
- • Laser Treatments
- • Cosmetic Dermatology
Visit Our Offices
Services:
- • Medical Dermatology
- • Surgical Dermatology
- • Laser Treatments
- • Cosmetic Dermatology
Services:
- • Medical Dermatology
- • Surgical Dermatology
- • Laser Treatments
- • Cosmetic Dermatology